NEET SS 2024 DrNB Medical Genetics Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Medical Genetics Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Medical Genetics Paper 3 Question Paper | Check Solutions |

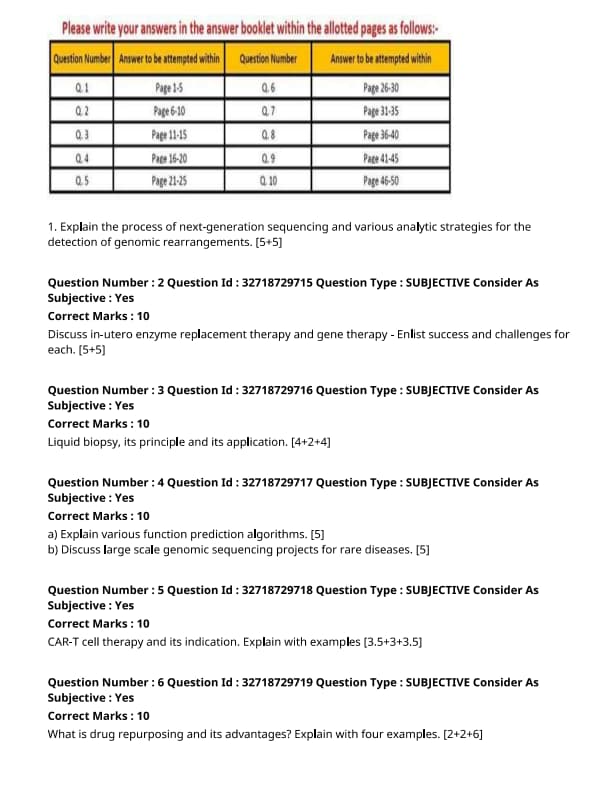
Explain the process of next-generation sequencing and various analytic strategies for the detection of genomic rearrangements.
Discuss in-utero enzyme replacement therapy and gene therapy - Enlist success and challenges for each.
Liquid biopsy, its principle and its application.
Explain various function prediction algorithms.
Discuss large scale genomic sequencing projects for rare diseases.
CAR-T cell therapy and its indication. Explain with examples.
What is drug repurposing and its advantages? Explain with four examples.
Preimplantation genetic diagnosis and its types.
Explain National Policy for Rare Disease (NPRD) of India.
Discuss associated challenges in implementation of the policy.
Explain haemopoietic stem cell transplantation.
Write 4 absolute indications amongst rare inherited disorders.




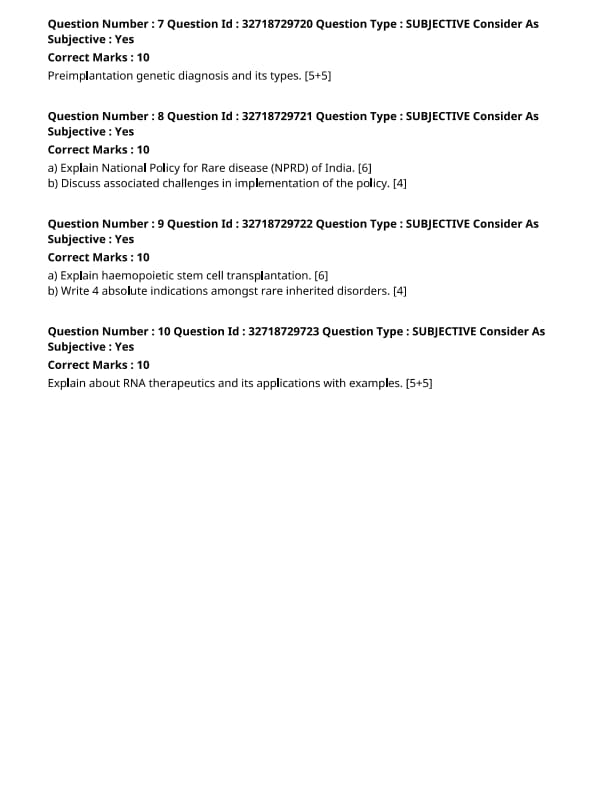

Comments