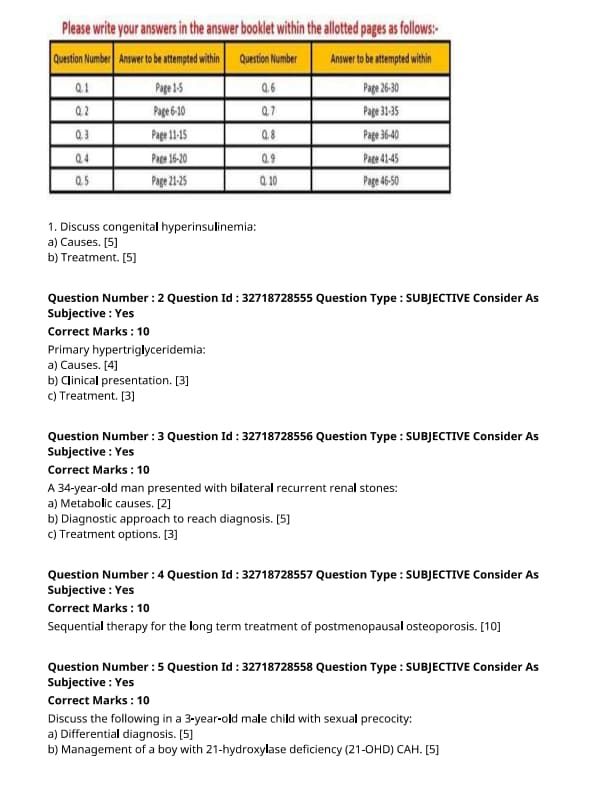
NEET SS 2024 DrNB Endocrinology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Endocrinology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Endocrinology Paper 3 Question Paper | Check Solutions |
Discuss causes of congenital hyperinsulinemia:
View Solution
Step 1: Overview of Congenital Hyperinsulinemia:
Congenital hyperinsulinemia is a rare disorder characterized by the inappropriate secretion of insulin, leading to persistent hypoglycemia in newborns and infants. It is caused by mutations that affect the regulation of insulin secretion.
Step 2: Causes of Congenital Hyperinsulinemia:
Congenital hyperinsulinemia can be caused by a variety of genetic mutations, including:
1. Beta-cell Mutations: Mutations in the genes that regulate insulin secretion, such as the ABCC8 and KCNJ11 genes, lead to inappropriate insulin release.
2. Familial Causes: In some cases, the condition runs in families, indicating a genetic predisposition.
3. Defective Sulfonylurea Receptor: Defects in the sulfonylurea receptor, which normally helps regulate insulin release, can cause persistent insulin secretion.
4. Congenital Hyperinsulinism Due to Epigenetic Changes: Some cases are caused by epigenetic modifications that lead to unregulated insulin secretion in the pancreas.
Quick Tip: Congenital hyperinsulinemia can be caused by genetic mutations in insulin secretion pathways, leading to persistent hypoglycemia in affected individuals.
Treatment of Congenital Hyperinsulinemia.
View Solution
Step 1: Medical Management:
1. Diazoxide: The first-line treatment for congenital hyperinsulinemia is diazoxide, which inhibits insulin release from the beta cells. It helps raise blood glucose levels in affected infants.
2. Octreotide: This somatostatin analog can also be used to inhibit insulin secretion when diazoxide is ineffective or contraindicated.
Step 2: Surgical Management:
In cases where medical management fails or if there is focal hyperinsulinism, surgery may be required.
1. Pancreatectomy: Partial pancreatectomy may be performed to remove the hyperinsulinic tissue, especially in cases where the condition is localized to one part of the pancreas.
2. Subtotal Pancreatectomy: In cases of diffuse hyperinsulinism, a more extensive surgery may be required, though it carries the risk of diabetes.
Step 3: Monitoring and Support:
Continuous monitoring of blood glucose levels is essential, and intravenous glucose may be required in the acute management phase.
Quick Tip: Diazoxide is the primary treatment for congenital hyperinsulinemia, but surgery may be needed if medical therapy fails.
Primary Hypertriglyceridemia:
Causes.
View Solution
Primary hypertriglyceridemia is a genetic condition characterized by high levels of triglycerides in the blood. The causes are typically related to inherited disorders.
Step 1: Genetic Factors:
1. Familial Hypertriglyceridemia: This is the most common inherited cause, resulting from a genetic mutation that affects lipid metabolism.
2. Familial Combined Hyperlipidemia: This condition involves elevated triglycerides and cholesterol levels, often due to multiple genetic factors.
3. Lipoprotein Lipase Deficiency: A rare inherited disorder that leads to a deficiency in the enzyme lipoprotein lipase, which is essential for triglyceride metabolism.
4. Apolipoprotein C-II Deficiency: This condition leads to impaired lipoprotein lipase function, resulting in high triglyceride levels. Quick Tip: Genetic testing can help identify inherited causes of hypertriglyceridemia, guiding treatment strategies.
Primary Hypertriglyceridemia:
Clinical presentation.
View Solution
Primary hypertriglyceridemia may present with various clinical features, depending on the severity of the condition.
Step 1: Mild to Moderate Hypertriglyceridemia:
- Often asymptomatic and may be detected incidentally during routine blood tests.
- Patients may experience mild fatigue, abdominal discomfort, or recurrent mild pancreatitis.
Step 2: Severe Hypertriglyceridemia:
- Can lead to acute pancreatitis, a serious and painful condition that requires immediate medical attention.
- May also present with eruptive xanthomas (yellowish deposits of fat under the skin), particularly on the arms, legs, and buttocks.
Step 3: Long-Term Complications:
- Chronic hypertriglyceridemia is associated with an increased risk of cardiovascular disease due to the associated dyslipidemia. Quick Tip: Regular monitoring of triglyceride levels is essential for early detection and management of primary hypertriglyceridemia.
Primary Hypertriglyceridemia:
Treatment.
View Solution
The treatment of primary hypertriglyceridemia involves a combination of lifestyle modifications and medications.
Step 1: Lifestyle Modifications:
1. Dietary Changes: A low-fat, low-carbohydrate diet can help reduce triglyceride levels.
2. Weight Loss: Losing weight, especially abdominal fat, can significantly reduce triglyceride levels.
3. Exercise: Regular physical activity can help lower triglycerides and improve overall lipid profile.
Step 2: Medications:
1. Fibrates: These drugs, such as fenofibrate, are the first-line treatment for lowering triglyceride levels.
2. Niacin: Niacin (vitamin B3) can lower triglycerides by reducing hepatic production of very low-density lipoprotein (VLDL).
3. Omega-3 Fatty Acids: Prescription omega-3 fatty acids, such as icosapent ethyl, are used to lower triglyceride levels in patients at risk of cardiovascular disease.
4. Statins: Although primarily used to lower cholesterol, statins may also help lower triglyceride levels in some patients.
Step 3: Severe Cases:
- In severe cases with very high triglycerides (>1000 mg/dL), plasmapheresis or insulin therapy may be considered to rapidly lower triglyceride levels and prevent acute pancreatitis.
Quick Tip: Managing primary hypertriglyceridemia early with lifestyle changes and medications can prevent complications such as pancreatitis and cardiovascular disease.
A 34-year-old man presented with bilateral recurrent renal stones:
Metabolic causes.
View Solution
Metabolic causes of recurrent bilateral renal stones are often related to disturbances in urine composition, which promote stone formation.
Step 1: Common Metabolic Causes:
1. Hypercalciuria: Excess calcium in the urine can lead to calcium oxalate stone formation. It may be due to dietary factors, hyperparathyroidism, or certain genetic conditions.
2. Hyperoxaluria: Increased excretion of oxalate in the urine, often caused by excessive dietary intake, malabsorption, or certain genetic disorders, can contribute to calcium oxalate stone formation.
3. Hyperuricosuria: High levels of uric acid in the urine can lead to uric acid stones, often associated with conditions like gout or high purine intake.
4. Hypocitraturia: Low levels of citrate in the urine reduce the ability to inhibit stone formation, leading to an increased risk of calcium-based stones.
5. Distal Renal Tubular Acidosis (RTA): This condition leads to acidic urine, which promotes the formation of calcium phosphate stones. Quick Tip: Metabolic disturbances like hypercalciuria, hyperoxaluria, and hypocitraturia are key factors in the development of recurrent kidney stones.
A 34-year-old man presented with bilateral recurrent renal stones:
Diagnostic approach to reach diagnosis.
View Solution
A thorough diagnostic approach is necessary to identify the underlying cause of recurrent renal stones and guide appropriate treatment.
Step 1: Clinical Evaluation:
1. History Taking: Detailed history of stone episodes, family history, dietary habits, and any underlying conditions (such as gout or gastrointestinal disease) is essential.
2. Physical Examination: Examining for signs of systemic diseases, such as hypertension, obesity, or bone disease, which may indicate underlying metabolic issues.
Step 2: Laboratory Tests:
1. Urinary Analysis: Urine tests for pH, calcium, oxalate, uric acid, and citrate levels to assess metabolic causes.
2. Serum Tests: Measuring serum calcium, phosphate, creatinine, and parathyroid hormone (PTH) levels. Elevated PTH may suggest hyperparathyroidism.
3. 24-Hour Urine Collection: A 24-hour urine collection helps assess calcium, oxalate, uric acid, and citrate levels in detail, providing valuable information on metabolic abnormalities.
Step 3: Imaging Studies:
1. Ultrasound: Non-invasive method to assess for kidney stones and renal damage.
2. CT Scan: A contrast-enhanced CT scan helps detect stones, their size, and location, as well as any obstructive complications.
3. X-rays: A KUB (kidneys, ureters, and bladder) X-ray may be useful for detecting radio-opaque stones.
Step 4: Specialized Tests:
1. Stone Analysis: If stones are passed or removed, analysis of the stone composition helps guide treatment.
2. Genetic Testing: For suspected inherited conditions such as cystinuria or primary hyperoxaluria. Quick Tip: A comprehensive approach combining clinical, laboratory, and imaging studies is crucial to identifying the metabolic cause of recurrent renal stones.
A 34-year-old man presented with bilateral recurrent renal stones:
Treatment options.
View Solution
The treatment of recurrent renal stones involves addressing both the acute episodes of stone formation and the underlying metabolic abnormalities to prevent recurrence.
Step 1: Medical Management:
1. Hydration: Ensuring adequate fluid intake to prevent dehydration and reduce urine concentration.
2. Dietary Modifications: Adjusting dietary intake, such as reducing oxalate-rich foods, limiting sodium and animal protein, and increasing citrate intake.
3. Medications:
- Thiazide Diuretics: For hypercalciuria, thiazide diuretics help reduce calcium excretion in the urine.
- Potassium Citrate: For hypocitraturia, potassium citrate increases urinary citrate, preventing stone formation.
- Allopurinol: For hyperuricosuria, allopurinol can reduce uric acid levels in the urine.
- Bicarbonate or Citrate Therapy: For metabolic acidosis associated with distal renal tubular acidosis.
Step 2: Surgical Management:
1. Lithotripsy: Shockwave lithotripsy (SWL) is used to break down stones into smaller pieces, making them easier to pass.
2. Endoscopic Stone Removal: Procedures like ureteroscopy and percutaneous nephrolithotomy (PCNL) are used to remove or fragment larger stones.
3. Open Surgery: Reserved for very large or complicated stones that cannot be treated with less invasive methods.
Step 3: Prevention:
1. Long-Term Medical Therapy: Patients with recurrent stones may require long-term medications, such as thiazides or potassium citrate, to prevent recurrence.
2. Lifestyle Modifications: Encourage regular physical activity, weight management, and avoidance of high-risk dietary habits. Quick Tip: Both medical therapy and lifestyle modifications are key components in preventing recurrent renal stones.
Sequential therapy for the long term treatment of postmenopausal osteoporosis.
View Solution
Sequential therapy for postmenopausal osteoporosis involves the use of different classes of medications over time to optimize the long-term management of the disease. The goal of sequential therapy is to reduce fracture risk and improve bone mineral density (BMD) while minimizing side effects and achieving a balance between efficacy and safety.
Step 1: Initial Treatment:
1. Bisphosphonates: The first line of treatment often involves bisphosphonates, such as alendronate, risedronate, or zoledronic acid. These drugs inhibit osteoclast-mediated bone resorption, increasing bone density and reducing fracture risk.
2. Denosumab: Another first-line therapy option is denosumab, a monoclonal antibody that targets RANKL, a protein essential for osteoclast activation. It helps in decreasing bone resorption and maintaining bone strength.
Step 2: Transition to Other Agents:
Once the patient has been on bisphosphonates or denosumab for a period (typically 3-5 years), a drug holiday or a switch to a different agent may be considered to reduce the risk of long-term side effects.
Step 3: Other Options in Sequential Therapy:
1. Anabolic Agents (e.g., Teriparatide or Abaloparatide): After prolonged use of antiresorptive therapies, anabolic agents may be used to stimulate new bone formation and improve BMD. These are particularly helpful in patients with severe osteoporosis or high fracture risk.
2. Selective Estrogen Receptor Modulators (SERMs): Medications like raloxifene can be considered for patients who are at risk of breast cancer or require additional anti-estrogenic effects.
Step 4: Monitoring and Adjustments:
Regular monitoring of bone mineral density, fracture risk, and the potential for side effects is essential in adjusting therapy. Sequential therapy may involve cycling between antiresorptive and anabolic agents, depending on the patient's response to treatment. Quick Tip: Sequential therapy is personalized based on patient risk factors and response to initial treatments, ensuring long-term efficacy and safety.
Discuss the following in a 3-year-old male child with sexual precocity:
Differential diagnosis
View Solution
Step 1: Definition of Sexual Precocity:
Sexual precocity refers to the early onset of secondary sexual characteristics in a child. In a 3-year-old male, this could involve the development of early signs of puberty, such as testicular enlargement, pubic hair growth, and increased levels of testosterone.
Step 2: Differential Diagnosis:
1. Central Precocious Puberty (CPP): This is caused by the early activation of the hypothalamic-pituitary-gonadal axis. It is typically idiopathic but can be caused by CNS tumors, infections, or trauma.
2. Peripheral Precocious Puberty: This occurs due to excess gonadal or adrenal steroid production, independent of the hypothalamic-pituitary-gonadal axis. Causes include:
- Congenital Adrenal Hyperplasia (CAH): CAH can lead to excess androgen production and early virilization.
- Gonadal Tumors: Tumors in the testes or ovaries can produce excess sex hormones.
3. Exogenous Hormone Exposure: Accidental or deliberate exposure to external sources of androgens, such as medications or creams, may cause precocious puberty.
Quick Tip: A thorough workup, including hormone assays and imaging, is crucial in differentiating between central and peripheral precocious puberty.
Discuss the following in a 3-year-old male child with sexual precocity:
Management of a boy with 21-hydroxylase deficiency (21-OHD) CAH.
View Solution
Step 1: Understanding 21-OHD CAH:
21-hydroxylase deficiency is the most common form of congenital adrenal hyperplasia (CAH) and leads to a defect in cortisol and aldosterone synthesis, causing an accumulation of androgens. This results in virilization of the external genitalia in females and precocious puberty in males.
Step 2: Management of 21-OHD CAH:
1. Glucocorticoid Therapy: The mainstay of treatment is the administration of glucocorticoids (e.g., hydrocortisone) to suppress excess adrenal androgen production.
- The goal is to replace cortisol, normalize growth, and prevent early puberty.
2. Mineralocorticoid Therapy: If there is salt-wasting (more common in severe forms of CAH), mineralocorticoids (e.g., fludrocortisone) are used to replace aldosterone and maintain sodium balance.
3. Monitoring: Regular monitoring of electrolytes, growth parameters, and adrenal function is essential. The patient may also need periodic adjustments to their medication based on clinical response and lab results.
4. Surgical Intervention: In cases of severe virilization in female infants, reconstructive surgery of the genitalia may be required.
5. Genetic Counseling: Parents of children with 21-OHD CAH should be counseled about the inherited nature of the condition and the risk to future children.
Quick Tip: Early diagnosis and appropriate management with glucocorticoid and mineralocorticoid therapy can help prevent the complications of 21-OHD CAH, including premature puberty and adrenal crisis.
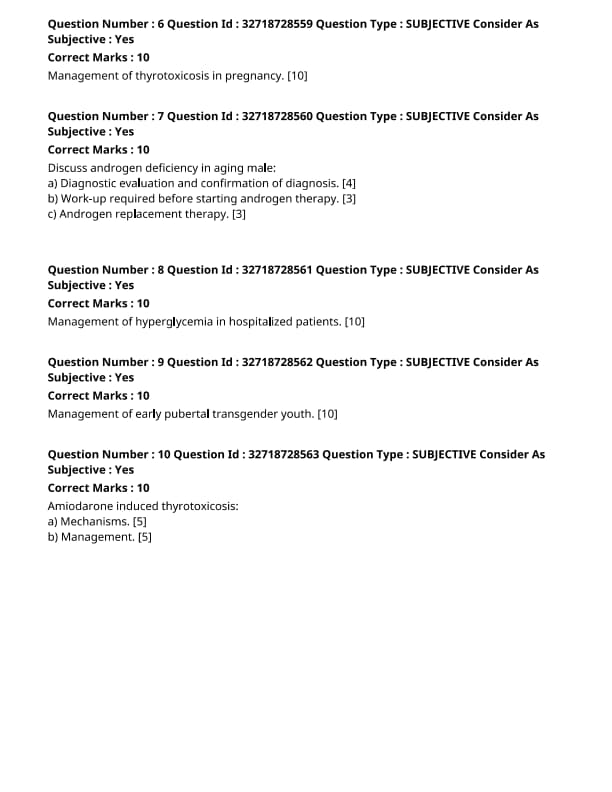
Management of thyrotoxicosis in pregnancy.
View Solution
Thyrotoxicosis in pregnancy refers to the clinical condition where there is an excess of thyroid hormone in the body, which can adversely affect both the mother and the fetus. The most common cause of thyrotoxicosis in pregnancy is Graves' disease, though it can also result from subacute thyroiditis, toxic multinodular goiter, or other thyroid conditions.
Step 1: Diagnosis of Thyrotoxicosis in Pregnancy:
1. Clinical Features: Symptoms include weight loss, palpitations, tremors, heat intolerance, and increased appetite. Pregnancy-specific symptoms may include hyperemesis gravidarum, as well as an increase in maternal heart rate and blood pressure.
2. Laboratory Tests: Blood tests to measure thyroid function (TSH, Free T4, and Free T3 levels) are essential. In pregnancy, TSH levels are generally lower due to the effects of human chorionic gonadotropin (hCG) on the thyroid gland. Thus, a low TSH with elevated Free T4 and Free T3 suggests thyrotoxicosis.
3. Ultrasound and Radioactive Iodine: A thyroid ultrasound may be used to detect goiter or nodules. Radioactive iodine scans are typically avoided during pregnancy due to their potential teratogenic effects.
Step 2: Treatment of Thyrotoxicosis in Pregnancy:
1. Antithyroid Medications: The first-line treatment involves antithyroid drugs such as propylthiouracil (PTU) or methimazole.
- Propylthiouracil (PTU) is preferred in the first trimester due to its lower risk of teratogenicity, whereas methimazole is more commonly used in the second and third trimesters, as PTU is associated with liver toxicity.
2. Beta-blockers: Beta-blockers such as propranolol can be used to manage symptoms such as tachycardia and tremors, but they should be used cautiously and in conjunction with antithyroid medications.
3. Surgical Intervention: Surgery may be considered in rare cases where antithyroid medications are ineffective or if there is a large goiter causing compression. This is typically avoided in the first trimester due to the risks of anesthesia and potential pregnancy complications.
4. Monitoring and Dose Adjustment: Close monitoring of thyroid function during pregnancy is essential. The dosage of antithyroid medications may need to be adjusted frequently due to changes in thyroid hormone levels during pregnancy.
Step 3: Management of Complications:
1. Thyroid Storm: Thyroid storm is a rare but life-threatening complication of severe thyrotoxicosis, characterized by fever, tachycardia, heart failure, and altered mental status. Immediate treatment with antithyroid drugs, supportive care, and beta-blockers is required.
2. Impact on Fetal Development: Untreated thyrotoxicosis during pregnancy can lead to complications such as preterm labor, low birth weight, and fetal hyperthyroidism. Proper management reduces the risk of these complications. Quick Tip: Early diagnosis and appropriate treatment of thyrotoxicosis in pregnancy are critical for reducing maternal and fetal morbidity and preventing complications like thyroid storm.
Discuss androgen deficiency in aging male:
Diagnostic evaluation and confirmation of diagnosis.
View Solution
Androgen deficiency in aging males is a condition characterized by low testosterone levels that affect physical and psychological well-being.
Step 1: Clinical Symptoms:
- Symptoms may include fatigue, decreased libido, erectile dysfunction, reduced muscle mass, depression, and osteoporosis.
- Screening for symptoms should be performed using validated questionnaires, such as the Androgen Deficiency in Aging Male (ADAM) questionnaire or the Aging Male Symptoms (AMS) scale.
Step 2: Blood Tests:
- The diagnosis is confirmed by measuring total serum testosterone levels. A low testosterone level is generally defined as below 300 ng/dL.
- Blood tests should be performed in the morning (7 AM to 10 AM) when testosterone levels are highest. If initial levels are low, confirmatory tests should be done on a separate day.
- Free testosterone levels can also be measured, especially in patients with obesity or altered binding proteins.
Step 3: Additional Testing:
- Measure luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels to differentiate between primary hypogonadism (testicular failure) and secondary hypogonadism (pituitary or hypothalamic dysfunction).
- Prolactin levels may also be measured to rule out pituitary disorders. Quick Tip: Confirm low testosterone levels with repeat testing before starting treatment, and consider other causes for symptoms.
Work-up required before starting androgen therapy.
View Solution
Before starting androgen therapy, several tests and evaluations are necessary to ensure that the treatment is safe and appropriate.
Step 1: Exclude Contraindications:
- Perform a digital rectal exam (DRE) and serum prostate-specific antigen (PSA) testing to rule out prostate cancer.
- Testosterone therapy is contraindicated in men with prostate cancer or breast cancer.
Step 2: Cardiovascular Risk Assessment:
- Evaluate cardiovascular health as testosterone therapy may increase the risk of cardiovascular events. This includes measuring cholesterol levels, assessing for hypertension, and evaluating for a history of heart disease.
Step 3: Hematocrit and Hemoglobin Levels:
- Measure hematocrit and hemoglobin to check for polycythemia, which can be induced by testosterone therapy. Elevated hematocrit levels can increase the risk of thromboembolic events.
Step 4: Liver Function Tests:
- Liver function tests should be performed as testosterone therapy can cause hepatic toxicity in rare cases, particularly with oral forms. Quick Tip: Ensure that there are no contraindications or elevated risks before initiating testosterone therapy.
Androgen replacement therapy.
View Solution
Androgen replacement therapy aims to restore normal testosterone levels and alleviate the symptoms of androgen deficiency.
Step 1: Routes of Administration:
1. Intramuscular Injections: Testosterone enanthate or cypionate are commonly used for injections, given every 1-2 weeks.
2. Transdermal Patches or Gels: Testosterone is applied daily to the skin, providing more consistent testosterone levels.
3. Pellets: Testosterone pellets are implanted subcutaneously and release testosterone over several months.
Step 2: Monitoring During Therapy:
- Monitor testosterone levels after starting therapy to ensure they reach the normal range (300-1000 ng/dL).
- Regular follow-up includes checking for side effects such as elevated hematocrit, prostate abnormalities, and cardiovascular symptoms.
Step 3: Adjustments and Side Effects:
- Adjust dosage based on clinical response and side effects. Common side effects include acne, gynecomastia, and mood changes.
- Ensure that there is no excessive increase in hematocrit levels, which could increase the risk of blood clots. Quick Tip: Close monitoring of testosterone levels and side effects is essential during androgen replacement therapy to ensure safety and efficacy.
Management of hyperglycemia in hospitalized patients.
View Solution
Managing hyperglycemia in hospitalized patients is crucial for preventing complications, such as infections, delayed wound healing, and poor overall recovery. Hyperglycemia is common in both diabetic and non-diabetic patients during hospitalization due to stress, infection, and medications.
Step 1: Monitoring Blood Glucose Levels:
1. Frequent Blood Glucose Testing: Blood glucose should be monitored frequently, especially in patients with known diabetes, those receiving corticosteroids, or patients with acute illness. Target glucose levels should be individualized, but general targets are 140-180 mg/dL for most hospitalized patients.
2. Continuous Glucose Monitoring: In critically ill patients, continuous glucose monitoring may be used for more accurate and timely adjustments.
Step 2: Insulin Therapy:
1. Basal-Bolus Insulin Regimen: A basal-bolus insulin regimen, which includes long-acting insulin for basal coverage and short-acting insulin for meal-related spikes, is commonly used in hospitalized patients.
2. Sliding Scale Insulin: A sliding scale insulin regimen can be used as a supplementary approach, though it is often less preferred compared to the basal-bolus regimen. It involves adjusting insulin doses based on the patient's current blood glucose level.
Step 3: Adjusting for Underlying Conditions:
1. Acute Illness: In cases of acute illness or surgery, insulin requirements may change due to stress hormones or medications. Insulin therapy should be adjusted accordingly to manage fluctuations in glucose levels.
2. Discontinuing Medications: Drugs such as corticosteroids, which can elevate blood glucose, should be carefully monitored. If possible, non-glucose-elevating alternatives should be considered.
Step 4: Education and Long-Term Management:
1. Post-Discharge Care: Patients should be educated on proper glucose monitoring and insulin use upon discharge to prevent readmissions related to poorly controlled diabetes. Quick Tip: Effective glucose management requires close monitoring and individualized insulin therapy to reduce the risk of complications during hospitalization.
Mechanisms of Amiodarone-induced thyrotoxicosis.
View Solution
Step 1: Overview of Amiodarone-Induced Thyrotoxicosis (AIT):
Amiodarone-induced thyrotoxicosis is a form of thyroid dysfunction associated with the use of amiodarone, a drug commonly used for arrhythmias. AIT can be classified into two types: Type 1 and Type 2, each with different underlying mechanisms.
Step 2: Mechanisms of Type 1 AIT:
1. Excess Iodine Load: Amiodarone contains a large amount of iodine, which can lead to excessive thyroid hormone production in susceptible individuals, particularly in those with pre-existing thyroid abnormalities.
2. Thyroid Hormone Synthesis: The excess iodine can increase the synthesis and release of thyroid hormones, leading to hyperthyroidism.
Step 3: Mechanisms of Type 2 AIT:
1. Thyroiditis: Type 2 AIT is characterized by thyroid cell destruction caused by the toxic effects of amiodarone on the thyroid gland. This leads to the release of pre-formed thyroid hormones into the bloodstream, resulting in thyrotoxicosis.
2. Inflammation: Inflammation of the thyroid gland can lead to an acute increase in thyroid hormone levels, mimicking hyperthyroidism.
Quick Tip: Amiodarone-induced thyrotoxicosis can be classified into Type 1 (iodine-induced) and Type 2 (thyroiditis). Both require different management approaches.
Management of Amiodarone-induced thyrotoxicosis.
View Solution
Step 1: Approach to Management:
The management of amiodarone-induced thyrotoxicosis (AIT) depends on the type (Type 1 or Type 2) and the severity of the condition.
Step 2: Management of Type 1 AIT:
1. Discontinuation of Amiodarone: The first step in management is discontinuing amiodarone, as it is the primary causative agent.
2. Antithyroid Drugs: For Type 1 AIT, antithyroid drugs such as propylthiouracil (PTU) or methimazole can be used to block thyroid hormone synthesis.
3. Iodine Restriction: Avoiding iodine-containing substances and further iodine exposure is crucial in managing Type 1 AIT.
Step 3: Management of Type 2 AIT:
1. Corticosteroids: Type 2 AIT, being related to thyroiditis, is treated with corticosteroids (e.g., prednisone) to reduce thyroid inflammation and suppress the release of thyroid hormones.
2. Symptomatic Management: Beta-blockers may be used to control symptoms of hyperthyroidism, such as palpitations and tremors.
3. Thyroidectomy: In severe cases that do not respond to medical treatment, thyroidectomy may be considered, especially if the condition is causing significant symptoms or complications.
Quick Tip: Type 1 AIT is managed with antithyroid drugs, whereas Type 2 AIT is treated with corticosteroids to control inflammation and reduce thyroid hormone release.







Comments