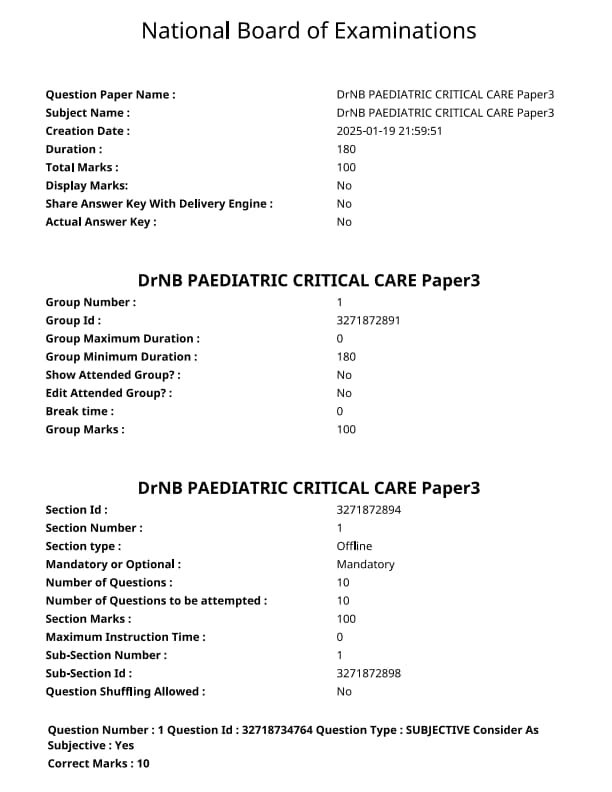
NEET SS 2024 DrNB Paediatric Critical Care Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Paediatric Critical Care Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Paediatric Critical Care Paper 3 Question Paper | Check Solutions |

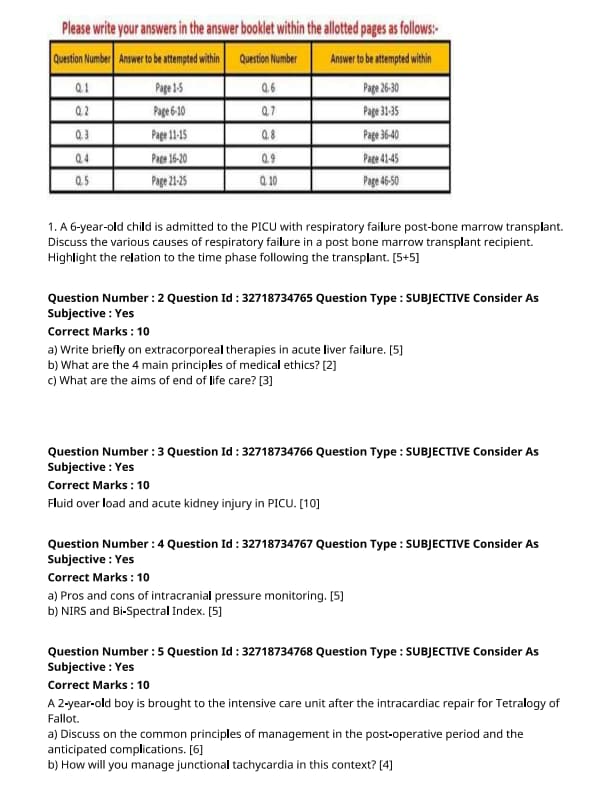
A 6-year-old child is admitted to the PICU with respiratory failure post-bone marrow transplant. Discuss the various causes of respiratory failure in a post bone marrow transplant recipient. Highlight the relation to the time phase following the transplant. [5+5]
View Solution
Respiratory failure in a post-bone marrow transplant (BMT) child can arise from several causes. These causes can be classified based on the time phase after the transplant. Understanding the timing and etiology is crucial for proper management.
Step 1: Causes of Respiratory Failure Early Post-Transplant (0-30 Days):
1. Infection: Early after the transplant, infections such as bacterial, viral (e.g., RSV, CMV), and fungal (e.g., Aspergillus) are common causes of respiratory failure due to immunosuppression.
2. Graft-versus-Host Disease (GVHD): GVHD affecting the lungs can lead to inflammation and lung damage, contributing to respiratory distress.
3. Acute Respiratory Distress Syndrome (ARDS): ARDS can be triggered by various factors such as infections, transfusions, or inflammation post-transplant.
Step 2: Causes of Respiratory Failure Late Post-Transplant (30 Days and Beyond):
1. Chronic Lung Disease (CLD): Chronic graft-versus-host disease can result in long-term pulmonary damage and lead to respiratory failure.
2. Infections: Late infections like pneumonia and opportunistic infections (e.g., fungal infections) can still occur due to immunosuppressive treatment.
3. Pulmonary Veno-occlusive Disease (PVOD): This is a rare but serious complication of BMT where blood vessels in the lungs become blocked, leading to respiratory failure.
Step 3: Relation to Time Phase:
- Early phase respiratory failure is primarily due to infections and ARDS.
- Late phase failure is more often caused by chronic GVHD, opportunistic infections, or PVOD. Quick Tip: Close monitoring of respiratory function and early intervention in the post-transplant period are critical to prevent long-term pulmonary complications.
Write briefly on extracorporeal therapies in acute liver failure.
View Solution
Extracorporeal therapies in acute liver failure (ALF) are interventions aimed at temporarily supporting liver function until the liver either recovers or a liver transplant is performed. These therapies help in removing toxins, excess fluids, and waste products that the liver can no longer filter due to its failure.
Step 1: Types of Extracorporeal Therapies:
1. Continuous Renal Replacement Therapy (CRRT): Used to manage fluid balance and remove waste products, especially in patients with acute renal failure.
2. Plasmapheresis: A process in which plasma is removed and replaced to remove harmful substances from the blood.
3. Molecular Adsorbent Recirculating System (MARS): A system that filters toxins from the blood using albumin dialysis. It helps in detoxifying the blood by removing albumin-bound substances.
4. Liver Dialysis: Similar to kidney dialysis, this therapy filters waste products from the blood, though it is not a long-term solution.
Step 2: Effectiveness and Limitations:
These therapies are only temporary measures and do not replace the liver's regenerative capabilities. They can stabilize patients and buy time for either recovery or liver transplant but are not curative on their own. Quick Tip: Extracorporeal therapies are essential in providing temporary relief in acute liver failure, but a liver transplant remains the definitive treatment.
What are the 4 main principles of medical ethics?
View Solution
The four main principles of medical ethics are guidelines for healthcare professionals to ensure the well-being of patients while maintaining professional integrity.
Step 1: The Four Principles:
1. Autonomy: Respecting the patient's right to make their own decisions regarding their healthcare, after being provided with all necessary information.
2. Beneficence: The obligation to act in the best interest of the patient, promoting their well-being and preventing harm.
3. Non-maleficence: The principle of "do no harm," ensuring that healthcare interventions do not cause unnecessary harm or injury to the patient.
4. Justice: Ensuring fairness in healthcare, distributing resources and care equally without discrimination.
Step 2: Application in Practice:
These principles guide healthcare providers in ethical decision-making, balancing individual rights with the needs of the community and ensuring high standards of care. Quick Tip: The four principles of medical ethics—autonomy, beneficence, non-maleficence, and justice—form the foundation for ethical practice in medicine.
What are the aims of end of life care?
View Solution
End-of-life care focuses on providing comfort and dignity to patients who are approaching the final stages of life. It involves addressing the physical, emotional, social, and spiritual needs of patients while also supporting their families.
Step 1: Aims of End of Life Care:
1. Pain and Symptom Management: Ensuring that the patient is as comfortable as possible by controlling pain, nausea, and other distressing symptoms.
2. Psychosocial Support: Offering emotional, psychological, and social support to the patient and their family to cope with the impending loss.
3. Respect for Patient’s Wishes: Ensuring that the patient’s preferences for care, including their wishes regarding life-sustaining treatments, are honored.
4. Support for Family: Providing support to the family before, during, and after the death of the loved one, including bereavement counseling.
Step 2: The Goal of End of Life Care:
The primary goal is to ensure that the patient’s last days are spent with as much comfort, peace, and dignity as possible, addressing both physical and emotional aspects of their end-of-life experience. Quick Tip: End-of-life care aims to provide comfort, dignity, and support to both patients and their families during the final stages of life.
Fluid overload and acute kidney injury in PICU.
View Solution
Fluid overload and acute kidney injury (AKI) are common issues faced in the Pediatric Intensive Care Unit (PICU), where critically ill children are treated. These conditions can have serious consequences if not managed properly.
Step 1: Fluid Overload in PICU:
1. Definition: Fluid overload refers to the excessive accumulation of fluids in the body, often due to intravenous fluid administration or impaired renal function.
2. Causes: The causes of fluid overload in the PICU can include improper fluid management, renal failure, or excessive use of medications that cause fluid retention.
3. Symptoms: Common symptoms include edema, respiratory distress, and weight gain.
Step 2: Acute Kidney Injury (AKI) in PICU:
1. Definition: AKI is characterized by a sudden decline in kidney function, leading to the retention of waste products and fluid imbalances.
2. Causes: In the PICU, AKI can be caused by various factors such as hypovolemia, sepsis, nephrotoxic medications, or inadequate perfusion to the kidneys.
3. Symptoms: Symptoms include decreased urine output, swelling, elevated blood urea nitrogen (BUN), and creatinine levels.
Step 3: Management Strategies:
1. Fluid Management: Careful monitoring and adjustment of fluid intake are crucial to avoid fluid overload. The use of diuretics may help manage excess fluid in some cases.
2. Renal Support: In cases of AKI, renal replacement therapy (RRT) may be necessary to support kidney function while the underlying cause is treated.
3. Monitoring: Continuous monitoring of kidney function, urine output, and fluid balance is essential in managing both conditions. Quick Tip: Proper fluid management and early recognition of AKI are critical to improving outcomes in critically ill children in the PICU.
Pros and cons of intracranial pressure monitoring.
View Solution
Intracranial pressure (ICP) monitoring is used to detect and manage patients with conditions that can lead to elevated ICP, such as traumatic brain injury, stroke, and brain tumors. The benefits of ICP monitoring include the early detection of increased ICP, enabling timely intervention to prevent brain damage.
Step 1: Pros of ICP Monitoring:
1. Early Detection of Raised ICP: Continuous monitoring can help identify dangerous increases in ICP before symptoms become life-threatening.
2. Guides Treatment Decisions: ICP measurements help clinicians decide on therapeutic interventions, including sedation, hyperosmolar therapy, or surgery.
3. Improved Patient Outcome: Timely detection and treatment of raised ICP can significantly improve patient prognosis, particularly in critical cases.
4. Objective Data: Provides quantitative data to guide clinical decision-making.
Step 2: Cons of ICP Monitoring:
1. Invasive Procedure: ICP monitoring requires the insertion of a catheter or sensor into the brain, which carries a risk of infection, hemorrhage, and other complications.
2. Limited by Equipment and Expertise: Not all hospitals have the necessary equipment or personnel with the expertise to perform and interpret ICP measurements.
3. False Readings: Inaccurate ICP measurements can occur due to improper placement of the sensor or malfunctioning equipment. Quick Tip: ICP monitoring is essential for managing patients with conditions that may lead to elevated intracranial pressure. However, it carries risks that must be weighed against the potential benefits.
NIRS and Bi-Spectral Index.
View Solution
Near Infrared Spectroscopy (NIRS) and the Bi-Spectral Index (BIS) are non-invasive monitoring techniques used in clinical settings to assess brain function, especially during surgery and critical care.
Step 1: Near Infrared Spectroscopy (NIRS):
NIRS is a technique that uses near-infrared light to measure the oxygenation of the brain. It is commonly used in neurocritical care and during surgeries, such as cardiac and brain surgery, to monitor cerebral oxygenation in real-time.
1. Advantages of NIRS:
- Non-invasive and continuous monitoring.
- Provides real-time data on cerebral oxygenation.
- Helps guide interventions in critically ill patients.
2. Limitations of NIRS:
- Sensitive to movement artifacts.
- Limited by tissue thickness and light absorption.
Step 2: Bi-Spectral Index (BIS):
The Bi-Spectral Index (BIS) is a measure of brain activity used primarily to monitor anesthetic depth during surgery. BIS is calculated from EEG signals and is a numerical value that helps anesthesiologists maintain an appropriate level of sedation.
1. Advantages of BIS:
- Provides a reliable measure of anesthetic depth.
- Helps prevent under- or over-sedation during surgeries.
- Reduces the use of excessive anesthetics.
2. Limitations of BIS:
- May not be accurate in patients with abnormal EEG patterns or high levels of muscle activity.
- Requires specialized equipment. Quick Tip: Both NIRS and BIS are valuable tools for monitoring brain function and guiding therapeutic interventions, but each has its limitations that should be considered when choosing the appropriate method.
A 2-year-old boy is brought to the intensive care unit after the intracardiac repair for Tetralogy of Fallot.
Discuss on the common principles of management in the post-operative period and the anticipated complications.
View Solution
Step 1: Principles of Management in the Post-operative Period:
The post-operative management of a patient who has undergone intracardiac repair for Tetralogy of Fallot involves several key principles, including:
1. Monitoring: Continuous monitoring of vital signs, including heart rate, blood pressure, oxygen saturation, and respiratory status.
2. Pain Management: Adequate pain control is necessary to ensure comfort and prevent complications.
3. Cardiovascular Support: Management of fluid balance, inotropic support, and monitoring of cardiac output to maintain adequate perfusion.
4. Preventing Infection: Use of antibiotics as prophylaxis and maintaining strict aseptic technique to prevent surgical site infections.
5. Ventilation Support: Mechanical ventilation may be required to maintain proper oxygenation and carbon dioxide removal.
6. Gradual Mobilization: Early mobilization is encouraged to prevent complications like deep vein thrombosis and improve recovery.
Step 2: Anticipated Complications:
1. Arrhythmias: Post-operative arrhythmias, including atrial and ventricular arrhythmias, are common and may require pharmacologic or electrical management.
2. Heart Failure: Inadequate cardiac output or left ventricular dysfunction could lead to heart failure.
3. Pulmonary Complications: Atelectasis, pleural effusion, and pneumonia are potential risks that need to be monitored.
4. Infection: Surgical site infection, endocarditis, and sepsis remain potential complications.
5. Renal Dysfunction: Acute kidney injury could occur due to hypotension or nephrotoxic medications. Quick Tip: Post-operative care in pediatric cardiac surgery requires close monitoring and support to minimize complications and ensure optimal recovery.
A 2-year-old boy is brought to the intensive care unit after the intracardiac repair for Tetralogy of Fallot.
How will you manage junctional tachycardia in this context?
View Solution
Step 1: Understanding Junctional Tachycardia:
Junctional tachycardia is a type of arrhythmia that originates from the atrioventricular junction. It is characterized by a rapid heart rate, often above 100 beats per minute. In a post-operative patient, this condition could be triggered by the surgical procedure, hypoxia, electrolyte imbalances, or as a side effect of medications.
Step 2: Management of Junctional Tachycardia:
1. Stabilization: Ensure adequate oxygenation and ventilation, as hypoxia may worsen the arrhythmia.
2. Electrolyte Correction: Correct any electrolyte imbalances, particularly hypokalemia and hypomagnesemia, which can contribute to arrhythmias.
3. Vagal Maneuvers: Non-invasive techniques such as vagal maneuvers (e.g., ice to the face or carotid massage) may be attempted in some cases.
4. Pharmacologic Treatment: Adenosine is the first-line treatment for acute management of junctional tachycardia.
5. Antiarrhythmic Agents: If adenosine is not effective, other antiarrhythmic agents like amiodarone or procainamide may be used.
6. Electrocardioversion: In cases of severe or refractory tachycardia, synchronized cardioversion may be required. Quick Tip: Junctional tachycardia requires prompt recognition and management to prevent hemodynamic instability in post-operative pediatric patients.
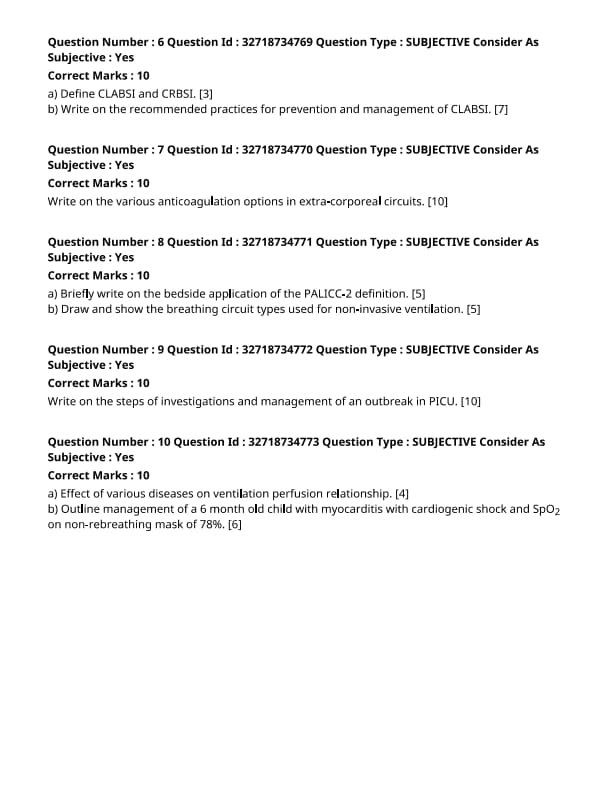
Define CLABSI and CRBSI. [3]
View Solution
Step 1: Definition of CLABSI:
CLABSI (Central Line-Associated Bloodstream Infection) is a type of bloodstream infection that occurs when bacteria or other pathogens enter the bloodstream through a central line, which is a catheter placed in a large vein, typically used for prolonged intravenous therapy.
Step 2: Definition of CRBSI:
CRBSI (Catheter-Related Bloodstream Infection) is an infection that is associated with the presence of a catheter in a blood vessel. It is diagnosed when the infection is directly related to the catheter and is confirmed through blood cultures. Quick Tip: Central lines should always be handled with sterile techniques to reduce the risk of CLABSI and CRBSI.
Write on the recommended practices for prevention and management of CLABSI. [7]
View Solution
Step 1: Prevention Practices for CLABSI:
1. Proper Hand Hygiene: Healthcare providers must wash their hands thoroughly before and after any contact with central lines.
2. Aseptic Technique: During the insertion, maintenance, and removal of central lines, strict aseptic techniques should be followed to avoid contamination.
3. Use of Chlorhexidine: Chlorhexidine is commonly used to clean the skin before the insertion of the catheter, which reduces the risk of infection.
4. Minimal Catheter Manipulation: Avoid unnecessary handling of the catheter to reduce the risk of contamination.
Step 2: Management Practices for CLABSI:
1. Prompt Removal of the Catheter: If CLABSI is suspected, the catheter should be promptly removed to prevent further infection.
2. Antibiotic Therapy: Empiric antibiotic therapy should be initiated immediately upon diagnosis, followed by the appropriate targeted therapy based on blood culture results.
3. Close Monitoring: Patients should be closely monitored for signs of sepsis or any complications arising from CLABSI, and timely interventions should be made. Quick Tip: Prevention of CLABSI focuses on minimizing the risk of infection during catheter insertion, maintenance, and removal. Timely management is key to reducing morbidity.
Write on the various anticoagulation options in extracorporeal circuits.
View Solution
Anticoagulation in extracorporeal circuits is crucial to prevent blood clotting during procedures like hemodialysis, ECMO, and plasmapheresis. These circuits come in contact with foreign materials, which can trigger coagulation, leading to clot formation and circuit failure.
Step 1: Anticoagulation Methods:
1. Heparin: The most commonly used anticoagulant in extracorporeal circuits. It works by inhibiting thrombin and other clotting factors. Low-dose heparin is used to prevent clot formation, while high-dose heparin can be used in therapeutic situations.
2. Low-Molecular-Weight Heparin (LMWH): These are derivatives of heparin and have a more predictable anticoagulant effect. LMWH is less likely to cause bleeding complications compared to unfractionated heparin.
3. Direct Thrombin Inhibitors: Drugs like bivalirudin and argatroban directly inhibit thrombin and are used in patients who have heparin-induced thrombocytopenia (HIT) or other heparin-related issues.
4. Citrate: Citrate works by chelating calcium, which is necessary for the coagulation cascade. It is commonly used in renal replacement therapy and ECMO, particularly in patients with heparin allergies or HIT. Citrate requires careful monitoring to prevent metabolic disturbances like alkalosis or hypocalcemia.
Step 2: Monitoring and Adjustments:
Regular monitoring of activated partial thromboplastin time (aPTT) for heparin and ionized calcium levels for citrate is essential to prevent over-anticoagulation or under-anticoagulation.
Step 3: Challenges and Considerations:
1. Risk of Bleeding: Excessive anticoagulation can lead to bleeding complications, which is a significant concern in critically ill patients.
2. Management of Anticoagulation: Adjustments in dosing may be needed based on patient condition, the type of extracorporeal procedure, and the risk of clot formation versus bleeding. Quick Tip: Careful monitoring of anticoagulation levels in extracorporeal circuits is essential to balance the risk of clot formation and bleeding.
Briefly write on the bedside application of the PALICC-2 definition.
View Solution
The PALICC-2 definition (Pediatric Acute Lung Injury and Sepsis Consensus Conference) focuses on pediatric acute lung injury and its management in critically ill children. It provides guidelines to improve outcomes in pediatric intensive care units (PICU) by standardizing the diagnosis and management strategies for respiratory failure and sepsis in children.
Step 1: Bedside Application of PALICC-2:
1. Early Identification: The PALICC-2 helps in the early identification of pediatric patients who are at risk for acute respiratory distress syndrome (ARDS) and sepsis, which is critical for timely intervention.
2. Management Guidelines: It provides evidence-based guidelines for ventilatory support, fluid management, and infection control, which are essential in managing critically ill pediatric patients.
3. Targeted Monitoring: The definition emphasizes the importance of continuous monitoring of oxygenation, ventilation, and fluid status to tailor the therapeutic approach for individual patients.
4. Multidisciplinary Approach: Implementation of PALICC-2 involves a collaborative effort among PICU teams, including intensivists, nurses, and respiratory therapists, to manage complex cases effectively. Quick Tip: The PALICC-2 definition provides a structured approach to managing respiratory failure and sepsis in pediatric patients, improving clinical outcomes.
Draw and show the breathing circuit types used for non-invasive ventilation.
View Solution
Non-invasive ventilation (NIV) is a method of providing respiratory support without the need for intubation. Different breathing circuits are used based on the type of NIV, such as Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Airway Pressure (BiPAP).
Step 1: Types of Breathing Circuits for NIV:
1. CPAP Circuit: A CPAP circuit provides continuous positive airway pressure to keep the airways open. It consists of a mask, tubing, and a CPAP device that delivers constant airflow throughout the breathing cycle.
2. BiPAP Circuit: A BiPAP circuit provides two levels of pressure: higher pressure during inspiration (IPAP) and lower pressure during expiration (EPAP). The circuit includes a mask, tubing, and a BiPAP machine that automatically adjusts the pressure based on the patient's breathing pattern.
Step 2: Circuit Components:
1. Mask: The mask is placed over the nose or both the nose and mouth, delivering the prescribed pressure. Different mask types (full face, nasal, etc.) are used based on patient comfort and condition.
2. Tubing: Flexible tubes connect the mask to the CPAP or BiPAP device. The tubing delivers the air from the machine to the patient's airways.
3. Pressure Generator: The CPAP or BiPAP device acts as the pressure generator, ensuring that the required airway pressure is maintained throughout the breathing cycle. Quick Tip: Non-invasive ventilation circuits, such as CPAP and BiPAP, are essential for managing patients with respiratory distress without the need for intubation.
Write on the steps of investigations and management of an outbreak in PICU.
View Solution
An outbreak in a Pediatric Intensive Care Unit (PICU) is a serious concern that requires immediate investigation and management to prevent further spread and ensure the safety of vulnerable patients. The investigation and management of an outbreak typically involve the following steps:
Step 1: Identification of the Outbreak:
1. Case Identification: Identify the affected patients who present with similar symptoms or signs of infection. This could include surveillance for unusual increases in certain conditions like fever, respiratory distress, or gastrointestinal issues.
2. Assessment of the Spread: Determine the pattern of the outbreak (e.g., nosocomial infections, patient-to-patient transmission) and its timeline to understand the scope.
Step 2: Investigation of the Cause:
1. Clinical Examination: Perform detailed clinical examinations and laboratory investigations, including blood cultures, viral and bacterial cultures, and other relevant diagnostic tests.
2. Environmental Investigation: Check the PICU environment for potential sources of infection, such as contaminated equipment, air handling systems, or sanitation practices.
Step 3: Implementing Control Measures:
1. Isolation of Affected Patients: Isolate patients who are showing signs of the outbreak to prevent cross-contamination.
2. Infection Control Protocols: Reinforce or implement infection control measures such as strict hand hygiene, personal protective equipment (PPE) usage, and cleaning and disinfection of equipment.
3. Staff Monitoring: Monitor healthcare workers for signs of illness and ensure adherence to safety protocols.
Step 4: Management of Affected Patients:
1. Symptomatic Treatment: Provide supportive care, such as oxygen therapy, fluids, and medications for symptomatic relief.
2. Targeted Antimicrobial Therapy: Administer appropriate antibiotics, antivirals, or antifungals based on the identified pathogen.
3. Nutritional Support: Ensure the provision of adequate nutrition to the affected patients, as their immune system may be compromised.
Step 5: Communication and Documentation:
1. Internal Communication: Ensure clear communication between healthcare teams, infection control specialists, and hospital management.
2. Public Health Reporting: Report the outbreak to relevant health authorities for further investigation and support, especially if it involves a reportable infectious disease.
Step 6: Post-Outbreak Review and Prevention:
1. Outbreak Review: After the outbreak is under control, conduct a review to evaluate the effectiveness of the response and identify areas for improvement.
2. Long-Term Preventive Measures: Implement preventive measures to reduce the likelihood of future outbreaks, including ongoing surveillance, regular training for healthcare workers, and improvement in hospital infection control protocols. Quick Tip: Prompt identification and control of outbreaks in the PICU are critical to preventing the spread of infections in vulnerable pediatric patients. Strict adherence to infection control protocols and effective communication are essential.
Effect of various diseases on ventilation perfusion relationship.
View Solution
Step 1: Understanding Ventilation-Perfusion (V/Q) Relationship:
The V/Q ratio refers to the ratio of ventilation (air reaching the alveoli) to perfusion (blood flow to the alveoli). A normal V/Q ratio is approximately 0.8, indicating adequate matching of ventilation and perfusion.
Step 2: Effect of Diseases on V/Q Relationship:
1. Obstructive Pulmonary Diseases: In conditions such as asthma, chronic obstructive pulmonary disease (COPD), or emphysema, the ventilation to the alveoli is reduced, leading to a V/Q mismatch. This results in decreased oxygenation of the blood.
2. Restrictive Pulmonary Diseases: Diseases like pulmonary fibrosis and pneumonia limit lung expansion, reducing ventilation, but perfusion may remain normal or near normal, leading to a V/Q mismatch with decreased oxygenation.
3. Pulmonary Embolism: A blockage in the pulmonary arteries leads to reduced perfusion to certain areas of the lung, while ventilation remains normal, resulting in high V/Q ratios in affected areas.
4. Shunt: In conditions such as atelectasis or pneumonia, perfusion occurs in areas of the lung that are not ventilated, resulting in low V/Q ratios and hypoxia. Quick Tip: A V/Q mismatch can lead to hypoxemia, and understanding its pathophysiology is crucial for managing diseases like COPD, pulmonary embolism, and pneumonia.
Outline management of a 6-month-old child with myocarditis with cardiogenic shock and SpO2 on non-rebreathing mask of 78%.
View Solution
Step 1: Initial Management of Cardiogenic Shock:
The management of a child with myocarditis and cardiogenic shock includes immediate stabilization:
1. Oxygenation: Ensure adequate oxygenation using a non-rebreathing mask. A SpO2 of 78% is critically low and requires immediate action. Consider endotracheal intubation and mechanical ventilation if the child remains hypoxic.
2. Fluid Resuscitation: Careful fluid resuscitation is necessary to optimize cardiac output. However, fluid overload must be avoided due to the risk of worsening heart failure.
3. Inotropic Support: Medications such as dopamine or dobutamine are used to support cardiac function and improve perfusion.
4. Monitoring: Continuous monitoring of vital signs, urine output, and cardiac function (e.g., using an echocardiogram or central venous pressure) is essential.
Step 2: Pharmacologic Management:
1. Vasodilators: If the blood pressure is adequate, vasodilators (e.g., nitroprusside) may be considered to reduce afterload and improve cardiac output.
2. Antibiotics: If there is a concern for infection contributing to myocarditis, appropriate antibiotics should be started.
3. Steroids or Immunosuppressants: In cases of autoimmune myocarditis, steroids or other immunosuppressive therapies may be considered based on the underlying cause.
Step 3: Supportive Care:
1. Nutritional Support: Adequate nutritional support should be provided, especially in critically ill children.
2. Monitor for Complications: Continuous monitoring for arrhythmias, organ dysfunction (renal or hepatic), and worsening heart failure is critical. Quick Tip: Cardiogenic shock in pediatric myocarditis requires prompt intervention with oxygenation, inotropic support, and careful fluid management to prevent worsening of the condition.




Comments