NEET SS 2024 DrNB Paediatric Cardiology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Paediatric Cardiology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Paediatric Cardiology Paper 3 Question Paper | Check Solutions |
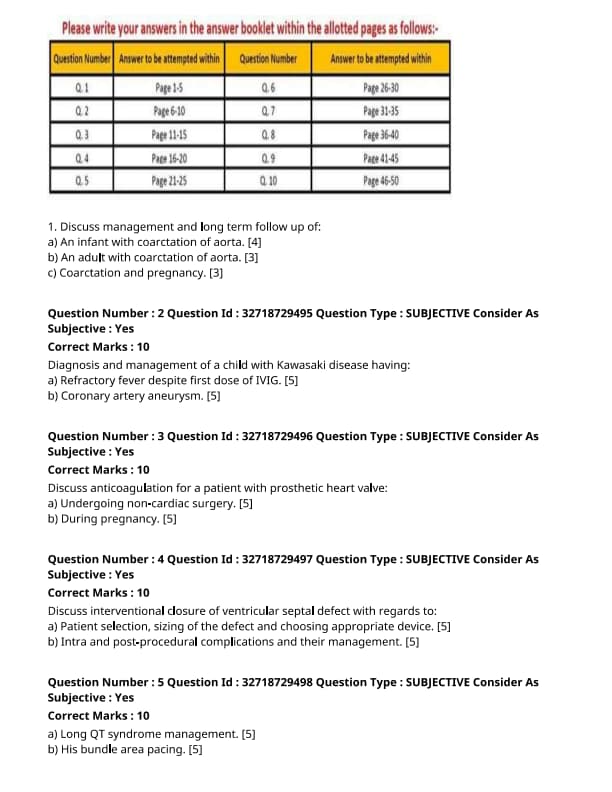
Discuss management and long term follow-up of:
An infant with coarctation of aorta. [4]
View Solution
Step 1: Initial Management of Coarctation in an Infant:
1. Prostaglandin E1 (PGE1): Initially, PGE1 is administered to keep the ductus arteriosus patent and improve systemic blood flow.
2. Surgical Intervention: Early surgical correction is necessary for infants, as coarctation can cause significant cardiovascular strain and failure. The surgery typically involves resection of the narrowed section and end-to-end anastomosis.
3. Balloon Angioplasty: In some cases, balloon angioplasty can be used as a less invasive treatment, though it may not be a permanent solution in all infants.
Step 2: Long-Term Follow-Up:
1. Blood Pressure Monitoring: After surgery, regular blood pressure monitoring is essential as some infants may develop hypertension due to residual stenosis or collateral vessels.
2. Cardiac Monitoring: Periodic echocardiograms and follow-up visits are crucial to assess the function of the heart and check for any complications such as re-coarctation.
3. Growth and Developmental Assessments: Monitoring the child's growth and overall development is important as coarctation may impact early development. Quick Tip: Early surgical intervention significantly improves outcomes in infants with coarctation of the aorta.
Discuss management and long term follow-up of:
An adult with coarctation of aorta. [3]
View Solution
Step 1: Management of Coarctation in Adults:
1. Surgical or Endovascular Repair: The treatment of choice is either surgical resection or endovascular stenting. Stenting is typically preferred in adults due to its minimally invasive nature.
2. Blood Pressure Control: Hypertension is a common issue, and it should be controlled using antihypertensive medications, especially beta-blockers, ACE inhibitors, or calcium channel blockers.
3. Cardiac Monitoring: Regular follow-up with echocardiograms and MRI is important to assess for complications such as re-coarctation or aneurysm formation.
Step 2: Long-Term Follow-Up:
1. Blood Pressure Management: Regular blood pressure monitoring is required to detect and manage hypertension post-surgery.
2. Cardiovascular Health: Periodic check-ups to evaluate heart function and the risk of other complications are crucial for long-term health. Quick Tip: For adults, early diagnosis and intervention are essential to prevent complications such as heart failure and stroke.
Discuss management and long term follow-up of:
Coarctation and pregnancy. [3]
View Solution
Step 1: Risks of Coarctation in Pregnancy:
1. Hypertension: Coarctation of the aorta can lead to severe pregnancy-related hypertension, including preeclampsia, which can complicate both the pregnancy and delivery.
2. Preterm Delivery: The increased cardiovascular strain may lead to preterm labor and delivery due to fetal distress.
3. Aneurysm Rupture: The pressure overload can increase the risk of aortic dissection or aneurysm rupture, which can be life-threatening.
Step 2: Management During Pregnancy:
1. Pre-conception Counseling: It is crucial for women with coarctation to receive pre-conception counseling to assess the risks and plan the pregnancy.
2. Blood Pressure Control: Tight control of blood pressure is essential throughout the pregnancy. Antihypertensive medications should be used carefully to avoid harm to the fetus.
3. Monitoring: Close monitoring of maternal and fetal well-being is necessary, including frequent blood pressure checks, echocardiograms, and ultrasounds to assess fetal growth. Quick Tip: Managing blood pressure and monitoring for complications is crucial for pregnant women with coarctation of the aorta.
Diagnosis and management of a child with Kawasaki disease having:
Refractory fever despite first dose of IVIG in Kawasaki disease.
View Solution
Refractory fever in Kawasaki disease (KD) is defined as persistent fever despite the first dose of intravenous immunoglobulin (IVIG). This is a challenging scenario and often requires further treatment to prevent coronary artery complications.
Step 1: Causes of Refractory Fever:
1. Incomplete Response to IVIG: Some children may have a partial or poor response to IVIG, leading to continued fever. Factors influencing response include delayed administration or severity of the disease.
2. Concurrent Infections: Bacterial or viral infections might coexist, leading to fever despite appropriate IVIG therapy.
3. Dosing Issues: Insufficient IVIG dose or improper administration technique may result in inadequate plasma levels of immunoglobulin.
Step 2: Management Options:
1. Second Dose of IVIG: If fever persists despite the first dose, a second dose of IVIG is often given.
2. Corticosteroids: Steroids are considered in cases where the fever persists after a second IVIG dose. They are used to reduce inflammation and improve outcomes.
3. Infliximab: This biologic agent, an anti-TNF antibody, may be used in cases that do not respond to multiple IVIG doses or steroids.
Step 3: Complications:
Refractory fever may indicate a risk for coronary artery abnormalities, including coronary artery aneurysms, requiring close monitoring and additional therapy. Quick Tip: Early recognition and treatment of refractory fever in Kawasaki disease are critical to prevent long-term cardiovascular complications.
Diagnosis and management of a child with Kawasaki disease having:
Coronary artery aneurysm in Kawasaki disease.
View Solution
Coronary artery aneurysms (CAA) are a major complication of Kawasaki disease (KD) and represent the most serious risk for cardiovascular morbidity and mortality in affected children.
Step 1: Pathophysiology:
1. Vascular Inflammation: In Kawasaki disease, inflammation of the arterial walls leads to weakening of the vessel walls, making them prone to dilatation and aneurysm formation.
2. Coronary Artery Involvement: The coronary arteries are most commonly affected, leading to dilation, thrombosis, or rupture.
3. Risk Factors: Factors such as delayed treatment with IVIG, age under one year, and male gender increase the risk of developing coronary artery aneurysms.
Step 2: Diagnosis:
1. Echocardiography: The primary diagnostic tool to evaluate coronary artery dilation and aneurysm formation. Repeat imaging may be required to monitor changes.
2. Coronary Angiography: In cases of severe aneurysms or uncertain findings, coronary angiography can provide detailed information about the extent of coronary involvement.
Step 3: Management and Prognosis:
1. IVIG Therapy: Early treatment with IVIG helps reduce the incidence of coronary artery aneurysms.
2. Aspirin: Low-dose aspirin is used for antiplatelet therapy to prevent thrombosis in affected arteries.
3. Surgical Intervention: In severe cases, coronary artery bypass grafting or stenting may be needed to manage large aneurysms and prevent rupture.
Step 4: Long-Term Follow-Up:
Children with coronary artery aneurysms need long-term follow-up to monitor for potential complications such as myocardial infarction or sudden death. Quick Tip: Early diagnosis and treatment of Kawasaki disease are crucial in preventing coronary artery aneurysms and associated complications.
Discuss anticoagulation for a patient with prosthetic heart valve :
undergoing non-cardiac surgery.
View Solution
Anticoagulation therapy is crucial for patients with prosthetic heart valves to prevent thromboembolic events. However, the management of anticoagulation during non-cardiac surgery requires careful consideration to balance the risk of thrombosis with the risk of bleeding.
Step 1: Preoperative Management:
1. Discontinuing Anticoagulation: In most cases, oral anticoagulants (such as warfarin) are stopped 5-7 days before surgery to allow the INR (International Normalized Ratio) to normalize.
2. Bridging Therapy: Patients with mechanical prosthetic heart valves may require bridging with low-molecular-weight heparin (LMWH) or unfractionated heparin (UFH) to prevent thromboembolism during the perioperative period.
3. Monitoring: Frequent monitoring of INR and anti-Xa levels is essential to ensure the proper therapeutic range during bridging therapy.
Step 2: Intraoperative Management:
1. Heparinization: Intraoperative heparinization is typically used to prevent clot formation, especially in surgeries with a high risk of bleeding. Heparin is usually discontinued before the end of the procedure.
2. Antidote Availability: In case of excessive bleeding, the availability of protamine sulfate, an antidote to heparin, should be ensured.
Step 3: Postoperative Management:
1. Resuming Anticoagulation: After surgery, anticoagulation is typically resumed as soon as possible, with bridging therapy continued until the patient is stable on warfarin therapy.
2. Patient-Specific Considerations: The decision to continue or adjust anticoagulation should be made based on the patient’s individual risk factors, such as the type of prosthetic valve and the nature of the surgery. Quick Tip: The management of anticoagulation during non-cardiac surgery in patients with prosthetic heart valves involves a balance between preventing thromboembolism and minimizing bleeding risk.
Discuss anticoagulation for a patient with prosthetic heart valve :
during pregnancy.
View Solution
Pregnancy in patients with prosthetic heart valves presents challenges in anticoagulation management due to the risks associated with both maternal and fetal health. Anticoagulation must be carefully managed to prevent thromboembolism while minimizing harm to the fetus.
Step 1: Considerations During Pregnancy:
1. Warfarin and Pregnancy: Warfarin is contraindicated during pregnancy, particularly in the first trimester, as it can cause fetal malformations and bleeding. It is usually discontinued and replaced with alternative therapies.
2. Heparin Use: Low-molecular-weight heparin (LMWH) is preferred during pregnancy due to its safety profile. It does not cross the placenta and is effective in preventing thromboembolic events.
3. Monitoring: Regular monitoring of anti-Xa levels is essential to ensure the appropriate anticoagulation effect with LMWH.
Step 2: Peripartum Management:
1. LMWH During Delivery: For labor and delivery, anticoagulation should be carefully managed. LMWH is typically stopped 24 hours before delivery, and the patient is closely monitored for signs of bleeding.
2. Postpartum Anticoagulation: After delivery, LMWH is continued until warfarin therapy can be safely resumed, typically after the postpartum period, to minimize the risk of bleeding.
Step 3: Individualized Approach:
The choice of anticoagulant and the management strategy should be individualized based on the type of prosthetic valve, the patient's clinical status, and the stage of pregnancy. Coordination with a multidisciplinary team, including obstetricians and cardiologists, is crucial. Quick Tip: Managing anticoagulation in pregnant patients with prosthetic heart valves requires a careful approach, with LMWH being the preferred anticoagulant during pregnancy.
Discuss interventional closure of ventricular septal defect with regards to:
Patient selection, sizing of the defect and choosing appropriate device.
View Solution
Interventional closure of a ventricular septal defect (VSD) is a minimally invasive procedure performed using a catheter to close the defect with an appropriate device, usually a septal occluder. The process requires careful consideration of patient selection, defect sizing, and choosing the appropriate device.
Step 1: Patient Selection:
1. Age and Size of the Patient: The procedure is typically indicated for patients who are older than 6 months, but the suitability depends on the patient’s overall health and the size of the defect.
2. Hemodynamics: Candidates must have clinically significant symptoms due to the VSD, such as failure to thrive, recurrent respiratory infections, or heart failure signs.
3. Associated Conditions: The patient should be free from other major congenital heart defects like pulmonary hypertension or significant aortic valve issues.
4. VSD Characteristics: The VSD should be of an appropriate size and location for device closure, usually a muscular or perimembranous VSD.
Step 2: Sizing the Defect:
1. Angiography and Echocardiography: Precise measurement of the defect size is performed using echocardiography or cardiac catheterization to assess the VSD diameter and shape.
2. Cardiac MRI or CT: In some cases, additional imaging like MRI or CT can be used to evaluate the anatomy of the VSD more thoroughly.
Step 3: Choosing the Appropriate Device:
1. Device Types: Several types of closure devices are available, including the Amplatzer VSD occluder and the occluder for muscular VSDs. The choice depends on the size and location of the defect.
2. Device Selection: The device must be selected based on the diameter of the VSD and the surrounding tissue structure. The device should be slightly larger than the defect to ensure a secure closure. Quick Tip: Careful patient selection, precise defect sizing, and the right device are essential for the successful interventional closure of a VSD.
Discuss interventional closure of ventricular septal defect with regards to:
Intra and post-procedural complications and their management.
View Solution
Interventional closure of a ventricular septal defect (VSD) is a relatively safe procedure; however, it carries the risk of certain complications both during and after the procedure. These complications require prompt identification and management to ensure a successful outcome.
Step 1: Intra-Procedural Complications:
1. Device Malposition: The device may be incorrectly placed or fail to fully occlude the VSD. This can be managed by repositioning or replacing the device.
2. Perforation of the Septum: There is a risk of septal perforation during device placement. This can be managed by withdrawing the device and using a new approach.
3. Arrhythmias: Arrhythmias may occur due to manipulation of the heart. These are usually transient and can be managed with antiarrhythmic drugs or temporary pacing.
Step 2: Post-Procedural Complications:
1. Device Embolization: The device may migrate from its initial position. This is a rare but serious complication that may require retrieval of the device via surgery or catheterization.
2. Infection: Endocarditis or other infections can occur. Prophylactic antibiotics are typically administered to reduce this risk.
3. Thrombosis and Stroke: There is a risk of thrombosis at the device site, potentially leading to embolism or stroke. Anticoagulation therapy may be used in some cases to prevent this.
4. Heart Block: A rare complication, especially in patients with perimembranous VSDs, where the conduction system may be affected, leading to heart block. This may require a pacemaker.
Step 3: Management of Complications:
1. Close Monitoring: After the procedure, patients should be closely monitored for complications such as arrhythmias, infection, or device-related issues.
2. Interventional or Surgical Correction: In the event of device malposition or embolization, additional interventions or surgical procedures may be required to correct the problem. Quick Tip: While interventional closure of VSD is generally safe, awareness and prompt management of complications are critical for successful outcomes.
Long QT syndrome management.
View Solution
Step 1: Understanding Long QT Syndrome:
Long QT syndrome is a condition where the heart's electrical system takes longer than normal to recharge between beats, leading to an increased risk of arrhythmias. It can be congenital or acquired.
Step 2: Management of Long QT Syndrome:
1. Avoid Triggers: The first step in managing long QT syndrome is identifying and avoiding potential triggers such as certain medications (e.g., antiarrhythmics, antibiotics), electrolyte imbalances (e.g., hypokalemia, hypomagnesemia), and stressful situations.
2. Beta-Blockers: Beta-blockers (e.g., propranolol) are the mainstay of treatment as they help prevent arrhythmias and lower the risk of sudden cardiac death.
3. Implantable Cardioverter Defibrillator (ICD): An ICD may be recommended for high-risk patients with a history of life-threatening arrhythmias or syncope. It detects arrhythmias and delivers shocks to restore normal rhythm.
4. Electrolyte Correction: Ensuring normal potassium and magnesium levels is essential in managing long QT syndrome, as electrolyte disturbances can exacerbate the condition.
5. Avoid Certain Medications: Medications that prolong the QT interval should be avoided whenever possible. Quick Tip: Beta-blockers and ICDs are critical components in managing high-risk patients with Long QT syndrome.
His bundle area pacing.
View Solution
Step 1: Understanding His Bundle Pacing:
His bundle pacing is a technique that involves placing a pacemaker lead at the His bundle, which allows for more physiologic conduction and synchrony compared to traditional ventricular pacing.
Step 2: Indications for His Bundle Pacing:
1. Bradycardia with Conduction System Disease: It is especially beneficial in patients with sick sinus syndrome or atrioventricular block.
2. Heart Failure: His bundle pacing has shown potential in improving ventricular synchrony, which can help in patients with heart failure who require pacing.
3. Preventing Long-Term Effects of Right Ventricular Pacing: His bundle pacing may be preferred over right ventricular pacing as it may reduce the risk of pacing-induced cardiomyopathy.
Step 3: Procedure:
1. Lead Placement: The pacing lead is inserted through a catheter and positioned at the His bundle using fluoroscopy.
2. Testing and Adjustment: Once the lead is in place, testing is done to confirm proper capture and threshold, ensuring the pacing is effective.
Step 4: Potential Complications:
1. Lead Displacement: There is a risk of lead displacement due to its delicate positioning at the His bundle.
2. Infection: As with any pacemaker placement, infection is a risk that needs to be managed.
3. Failure to Capture: The pacing lead may fail to capture the heart, requiring repositioning or replacement. Quick Tip: His bundle pacing offers a more physiologic form of pacing compared to traditional methods, especially in patients with conduction system diseases.
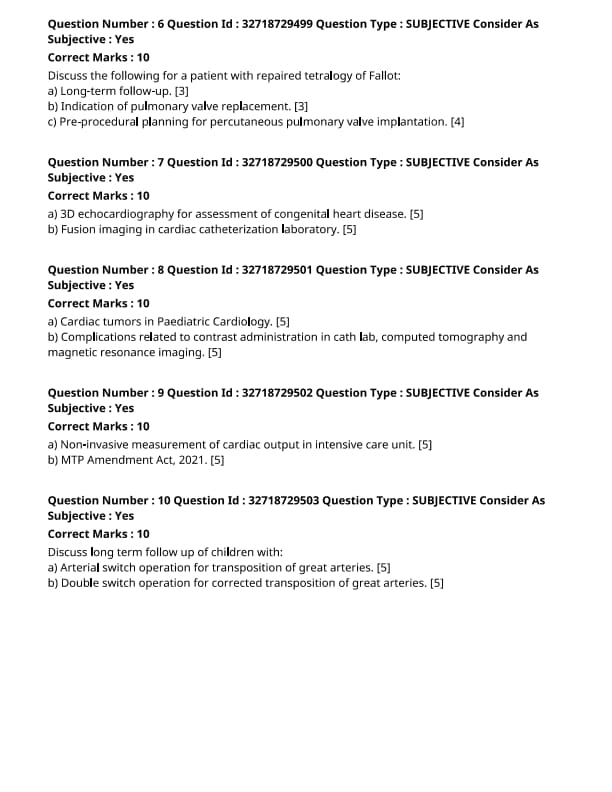
Discuss the following for a patient with repaired tetralogy of Fallot:
Long-term follow-up
View Solution
Step 1: Importance of Long-Term Follow-Up:
1. Cardiac Monitoring: Patients with repaired tetralogy of Fallot (TOF) should undergo lifelong cardiac follow-up, including regular echocardiograms, electrocardiograms (ECGs), and possibly MRI, to monitor for any residual defects or complications.
2. Assessment of Pulmonary Valve Function: Since pulmonary valve insufficiency is common after repair, follow-up should include evaluation of valve function and detection of any signs of right ventricular dysfunction.
3. Exercise and Lifestyle: Regular monitoring of exercise tolerance is important as patients may experience limitations due to residual heart defects or arrhythmias. Counseling on lifestyle modifications may also be necessary. Quick Tip: Ongoing follow-up is essential for detecting late complications, including arrhythmias, pulmonary valve dysfunction, and right ventricular issues.
Discuss the following for a patient with repaired tetralogy of Fallot:
Indication of pulmonary valve replacement
View Solution
Step 1: Pulmonary Valve Dysfunction in TOF:
1. Pulmonary Valve Regurgitation (PVR): The most common indication for pulmonary valve replacement (PVR) in TOF patients is significant pulmonary valve regurgitation, which can lead to right ventricular dilation and failure.
2. Right Ventricular Dysfunction: If the right ventricle becomes significantly enlarged or shows signs of failure due to prolonged pressure overload, pulmonary valve replacement is recommended to relieve stress on the right ventricle.
3. Exercise Intolerance: Severe exercise intolerance caused by pulmonary valve insufficiency or right heart failure may indicate the need for valve replacement. Quick Tip: Early intervention with pulmonary valve replacement can prevent irreversible right ventricular damage and improve quality of life.
Discuss the following for a patient with repaired tetralogy of Fallot:
Pre-procedural planning for percutaneous pulmonary valve implantation.
View Solution
Step 1: Patient Selection:
1. Anatomical Considerations: Patients must have adequate right ventricular size, and the pulmonary artery must be large enough to accommodate the valve.
2. Assessment of Valve Function: Pre-procedural imaging (usually MRI or CT) is essential to evaluate the pulmonary valve annulus and the condition of the right ventricle and pulmonary arteries.
3. Exclusion Criteria: Severe tricuspid valve regurgitation or significant arrhythmias may exclude patients from the percutaneous procedure and indicate the need for surgical intervention.
Step 2: Procedure Preparation:
1. Pre-procedural Imaging: MRI or CT scans are performed to assess the anatomy of the right ventricular outflow tract, pulmonary artery, and annulus for accurate valve sizing.
2. Anesthesia and Sedation: The procedure is usually performed under local anesthesia with sedation, and appropriate vascular access should be secured.
3. Device Selection: Sizing of the percutaneous pulmonary valve is based on pre-procedural imaging and patient anatomy. The right valve size and positioning must be carefully selected. Quick Tip: Accurate pre-procedural planning with imaging and careful patient selection is critical for the success of percutaneous pulmonary valve implantation.
3D echocardiography for assessment of congenital heart disease.
View Solution
3D echocardiography has revolutionized the assessment and management of congenital heart disease (CHD). It provides a three-dimensional visualization of cardiac structures, offering more detailed information than traditional 2D echocardiography.
Step 1: Advantages of 3D Echocardiography:
1. Detailed Visualization: It enables the assessment of complex congenital defects, including intracardiac anatomy, septal defects, and ventricular function.
2. Preoperative Planning: Surgeons can plan procedures more accurately by visualizing the heart in three dimensions, improving the outcome of surgeries.
3. Real-Time Imaging: 3D echocardiography allows for dynamic assessment of cardiac function, such as valve motion, myocardial deformation, and flow dynamics.
Step 2: Clinical Applications:
1. Assessment of CHD: It is used to diagnose and monitor congenital defects, including ventricular septal defects, atrial septal defects, and tetralogy of Fallot.
2. Assessment of Valve Function: 3D echocardiography helps in the evaluation of valve morphology and function in congenital heart disease, particularly in cases of valve stenosis or regurgitation.
Step 3: Limitations:
1. Technical Challenges: 3D echocardiography requires high-quality images, and obtaining clear views in some patients can be challenging.
2. Limited Availability: Not all healthcare facilities have the necessary equipment or expertise to perform 3D echocardiography. Quick Tip: 3D echocardiography provides a more detailed and accurate evaluation of congenital heart defects, aiding in both diagnosis and surgical planning.
Fusion imaging in cardiac catheterization laboratory.
View Solution
Fusion imaging combines multiple imaging modalities to improve the accuracy and safety of procedures in the cardiac catheterization laboratory. This technology integrates real-time fluoroscopy with other imaging techniques such as CT, MRI, and echocardiography.
Step 1: Benefits of Fusion Imaging:
1. Improved Precision: It enhances the visualization of complex coronary anatomy, making it easier to navigate catheters and stents during angioplasty or other interventions.
2. Reduced Radiation Exposure: By combining multiple imaging techniques, fusion imaging can reduce the need for prolonged fluoroscopy, thereby lowering radiation exposure to the patient and the medical team.
3. Enhanced Procedural Guidance: It allows for real-time guidance during procedures, helping physicians plan and execute interventions with greater accuracy and efficiency.
Step 2: Clinical Applications:
1. Coronary Artery Disease (CAD): Fusion imaging is useful in guiding interventions such as angioplasty and stenting in patients with CAD.
2. Congenital Heart Disease: It is also used to guide catheter-based interventions in patients with congenital heart disease, offering improved visualization of the vascular structures.
Step 3: Limitations:
1. Complexity of Setup: Fusion imaging systems require multiple modalities and expertise to operate effectively, which can be technically challenging.
2. Cost: The use of advanced imaging technologies increases the cost of procedures, limiting its availability in some settings. Quick Tip: Fusion imaging improves procedural accuracy and safety by combining different imaging techniques, making complex interventions easier to perform.
Cardiac tumors in Paediatric Cardiology.
View Solution
Cardiac tumors in pediatric patients are rare but can cause significant morbidity and mortality if not diagnosed and treated appropriately. The majority of cardiac tumors in children are benign, with a small percentage being malignant.
Step 1: Types of Cardiac Tumors in Pediatrics:
1. Rhabdomyomas: These are the most common primary cardiac tumors in children, often associated with tuberous sclerosis. They are usually benign and tend to regress over time.
2. Fibromas: These tumors are the second most common type and are often found in the ventricular myocardium. They can cause obstruction or arrhythmias.
3. Teratomas and Myxomas: These are less common and can be benign or malignant. Myxomas, though rare in children, can present with obstruction and embolic phenomena.
4. Malignant Tumors: These include sarcomas, which are aggressive and may present with heart failure, arrhythmias, or embolic events.
Step 2: Diagnosis:
1. Echocardiography: This is the primary diagnostic tool, allowing for the visualization of tumors, their location, and size.
2. Magnetic Resonance Imaging (MRI): MRI provides detailed information regarding the tumor's tissue characteristics and its relationship to adjacent structures.
3. CT Scan: CT scans are sometimes used to evaluate the extent of the tumor or to guide surgery.
4. Biopsy: In some cases, a biopsy is required to confirm the diagnosis, especially for malignant tumors.
Step 3: Treatment:
1. Surgical Resection: The primary treatment for symptomatic tumors or those causing obstruction is surgical removal.
2. Observation: Many benign tumors, such as rhabdomyomas, may be monitored over time, especially if they are asymptomatic.
3. Chemotherapy and Radiation: These may be required for malignant tumors or those that cannot be completely removed. Quick Tip: Early detection and proper management of cardiac tumors in children can improve outcomes and reduce the risk of complications.
Complications related to contrast administration in cath lab, computed tomography, and magnetic resonance imaging.
View Solution
Contrast agents are commonly used in diagnostic imaging to enhance the visibility of structures and blood vessels. However, the use of contrast agents can lead to several complications, especially in high-risk patients.
Step 1: Complications in the Cath Lab:
1. Contrast-Induced Nephropathy (CIN): This is a significant risk in patients with pre-existing renal dysfunction. CIN is characterized by a rise in serum creatinine following the administration of contrast media.
2. Allergic Reactions: Some patients may experience allergic reactions to contrast agents, ranging from mild symptoms such as urticaria to severe reactions like anaphylaxis.
3. Extravasation: This occurs when contrast media leaks into the surrounding tissues instead of the bloodstream, potentially causing tissue necrosis and swelling.
Step 2: Complications in Computed Tomography (CT):
1. Renal Impairment: Similar to the cath lab, CT scans with contrast can cause kidney damage, especially in patients with pre-existing kidney disease.
2. Thyroid Dysfunction: Iodinated contrast agents used in CT can affect thyroid function, leading to hyperthyroidism or hypothyroidism in some cases.
3. Hepatic Dysfunction: In rare cases, contrast agents can cause liver injury, especially in patients with underlying liver disease.
Step 3: Complications in Magnetic Resonance Imaging (MRI):
1. Nephrogenic Systemic Fibrosis (NSF): Gadolinium-based contrast agents used in MRI have been associated with NSF, a rare but severe condition that causes fibrosis of the skin and internal organs in patients with renal impairment.
2. Allergic Reactions: Gadolinium-based contrast agents can also cause allergic reactions, although they are less common than with iodinated contrast agents.
3. Severe Injection Site Reactions: Extravasation can also occur with MRI contrast, although it is less common than with iodinated contrast used in CT and angiography.
Step 4: Preventive Measures:
1. Hydration: Adequate hydration before and after the administration of contrast can reduce the risk of CIN and improve kidney function.
2. Pre-Contrast Screening: Screening for renal function, allergies, and other risk factors before the administration of contrast agents is essential.
3. Use of Low-Osmolar Contrast Agents: Choosing low-osmolar or iso-osmolar contrast agents can reduce the risk of complications such as CIN and allergic reactions. Quick Tip: Pre-contrast screening and careful monitoring during imaging procedures can help minimize the risk of complications related to contrast administration.
Non-invasive measurement of cardiac output in intensive care unit.
View Solution
Non-invasive measurement of cardiac output (CO) in the intensive care unit (ICU) is essential for monitoring and managing critically ill patients. Cardiac output refers to the volume of blood the heart pumps per minute, and accurate measurement is crucial for assessing cardiovascular function.
Step 1: Methods of Non-Invasive Measurement:
1. Doppler Ultrasound: Doppler ultrasound is commonly used in ICUs to measure blood flow velocity, which can be used to estimate cardiac output. It is based on the Doppler effect, where the frequency of sound waves is altered by moving red blood cells.
2. Impedance Cardiography: This method uses electrical impedance to measure the change in thoracic fluid volume with each heartbeat. The device is non-invasive and provides real-time cardiac output estimation.
3. Bioimpedance Analysis: Similar to impedance cardiography, bioimpedance uses electrical signals to assess body resistance and estimate cardiac output. It is often used for continuous monitoring in critically ill patients.
4. Pulse Contour Analysis: This technique involves analyzing the shape of the arterial pressure waveform to estimate cardiac output. It is often used in conjunction with other hemodynamic parameters.
Step 2: Advantages and Limitations:
1. Advantages:
- Non-invasive, minimizing the risk of complications associated with invasive methods.
- Continuous monitoring in real-time, providing valuable data for treatment decisions.
- Ease of use and quick setup, reducing the need for highly specialized personnel.
2. Limitations:
- Less accurate than invasive methods, particularly in patients with arrhythmias or extreme obesity.
- Limited applicability in patients with poor signal quality or those who are highly unstable. Quick Tip: Non-invasive measurement techniques are crucial for continuous cardiac output monitoring, but they may not be as precise as invasive methods in all clinical scenarios.
MTP Amendment Act, 2021.
View Solution
The Medical Termination of Pregnancy (MTP) Amendment Act, 2021, is a significant legal reform in India that expands the legal framework surrounding abortion. The amendment aims to provide more accessible and safer reproductive health services for women while ensuring that abortions are conducted within medically safe parameters.
Step 1: Key Provisions of the MTP Amendment Act, 2021:
1. Extended Limit for Termination: The amendment increases the upper gestational limit for permissible abortion from 20 weeks to 24 weeks for certain categories of women, including minors, survivors of sexual assault, and women with physical disabilities or fetal abnormalities.
2. Improved Access for Women: The Act allows women to seek abortion services without requiring spousal consent, thus protecting the autonomy and privacy of the woman seeking the procedure.
3. Regulation of Medical Professionals: The Act establishes clearer guidelines for who can perform abortions and ensures that only qualified medical professionals, such as doctors with specialized training, are allowed to conduct such procedures.
Step 2: Categories of Women Covered:
1. Vulnerable Women: The law considers vulnerable women, including minors and victims of sexual violence, by allowing them to terminate pregnancies up to 24 weeks.
2. Physical and Mental Health Conditions: Women whose pregnancies pose a threat to their physical or mental health are also provided greater legal access to abortion under the new law.
Step 3: Implementation and Regulations:
1. Safe and Regulated Abortions: The law emphasizes the importance of conducting abortions in safe, regulated environments such as licensed healthcare facilities to minimize health risks to the woman.
2. Counseling and Consent: Mandatory counseling and consent protocols are now in place to ensure that the woman is fully informed before undergoing the procedure. Quick Tip: The MTP Amendment Act, 2021, enhances women's rights and access to safe abortion services while maintaining a balance between reproductive health and ethical medical practices.
Discuss long-term follow-up of children with:
Arterial switch operation for transposition of great arteries.
View Solution
Step 1: Understanding Arterial Switch Operation (ASO):
The arterial switch operation is the gold standard procedure for treating transposition of the great arteries (TGA). In TGA, the aorta arises from the right ventricle, and the pulmonary artery arises from the left ventricle, resulting in a reversal of blood flow. The ASO involves switching the origins of the aorta and pulmonary artery to their correct positions.
Step 2: Long-Term Follow-Up After ASO:
1. Cardiac Function Monitoring: Patients require long-term follow-up to assess cardiac function, particularly for left ventricular function, as it may be affected by the procedure. Regular echocardiograms and ECGs are needed.
2. Pulmonary Arterial Pressure: Monitoring of pulmonary arterial pressures is important, as some patients may develop pulmonary hypertension.
3. Risk of Arrhythmias: There is an increased risk of arrhythmias, particularly after ASO, due to scar tissue from the surgery.
4. Growth and Development: Ensuring normal growth and development is important, as some children may experience developmental delays.
5. Psychosocial Support: Long-term psychosocial support is necessary to help patients adjust to living with a congenital heart condition. Quick Tip: Close follow-up is essential for early detection of complications like arrhythmias, left ventricular dysfunction, or pulmonary hypertension.
Discuss long-term follow-up of children with:
Double switch operation for corrected transposition of great arteries.
View Solution
Step 1: Understanding Double Switch Operation (DSO):
The double switch operation is performed for patients with corrected transposition of the great arteries (CTGA), where the atrioventricular and ventriculo-arterial connections are reversed. The procedure involves two main components: the Mustard or Senning procedure to baffle the venous return and the arterial switch to reposition the aorta and pulmonary artery.
Step 2: Long-Term Follow-Up After DSO:
1. Cardiac Function Monitoring: Long-term follow-up includes regular monitoring of cardiac function, especially the right ventricle, which is responsible for pumping systemic blood after the operation. Echocardiograms and ECGs are used to track function.
2. Right Ventricular Function: The right ventricle, which is the systemic ventricle after a double switch, may be at risk for dysfunction over time. Follow-up includes monitoring for signs of right ventricular failure.
3. Arrhythmias: Patients are at high risk for arrhythmias due to the abnormal atrial and ventricular connections, and they may need pacemaker implantation or other interventions to manage arrhythmias.
4. Pulmonary Function: Regular assessments of pulmonary function are necessary to detect any long-term pulmonary complications.
5. Psychosocial Support: As with the ASO, long-term psychosocial support is vital to help children and families manage the ongoing challenges of living with a congenital heart defect. Quick Tip: The double switch operation is complex and requires lifelong monitoring for complications like arrhythmias and right ventricular dysfunction.




Comments