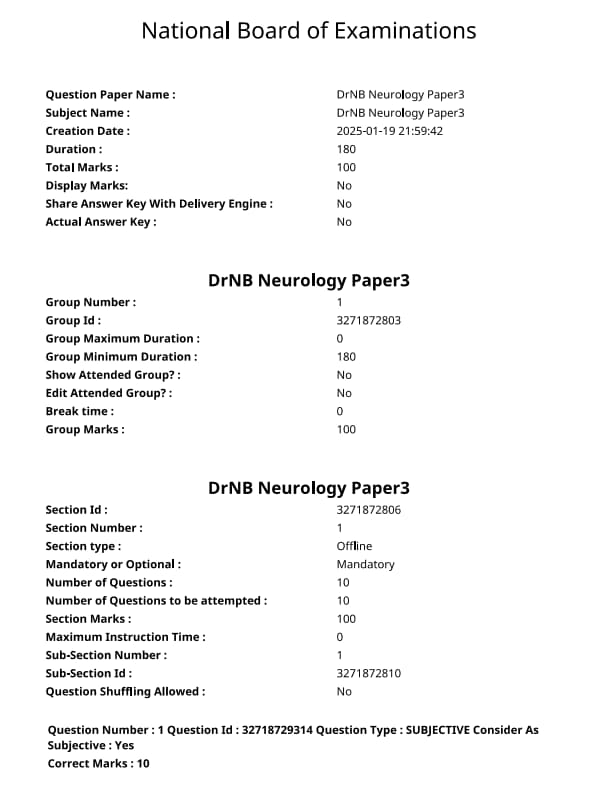
NEET SS 2024 DrNB Neurology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Neurology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Neurology Paper 3 Question Paper | Check Solutions |

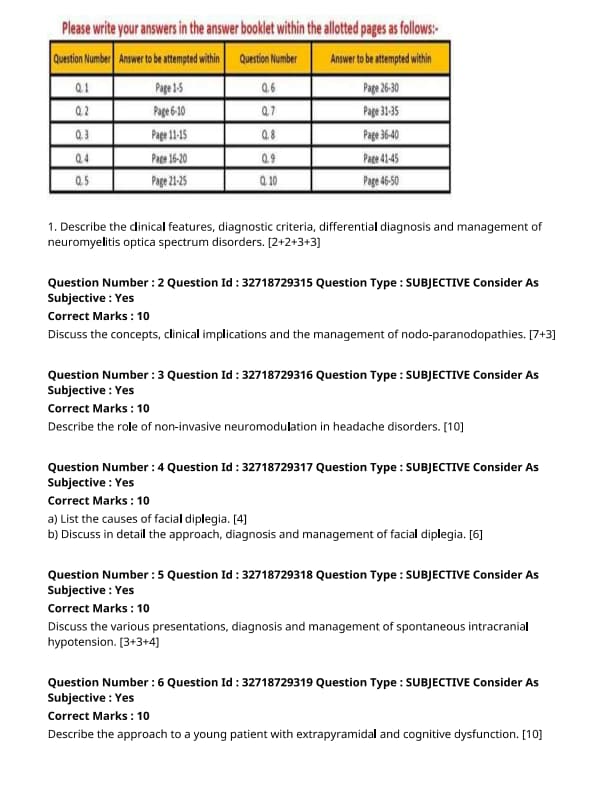
Describe the clinical features, diagnostic criteria, differential diagnosis, and management of neuromyelitis optica spectrum disorders.
View Solution
Neuromyelitis optica spectrum disorders (NMOSD) are a group of autoimmune demyelinating disorders primarily affecting the optic nerves and spinal cord. They are characterized by the presence of autoantibodies targeting aquaporin-4 (AQP4).
Step 1: Clinical Features:
1. Optic Neuritis: Acute vision loss in one or both eyes, often accompanied by pain on eye movement.
2. Transverse Myelitis: Sudden onset of weakness, sensory disturbances, and bowel or bladder dysfunction due to inflammation of the spinal cord.
3. Other Symptoms: Patients may also experience nausea, vomiting, respiratory failure, or seizures in severe cases.
Step 2: Diagnostic Criteria:
1. Serological Testing: Detection of anti-AQP4 antibodies is a hallmark of NMOSD, although a small percentage of patients may be seronegative.
2. MRI of the Brain and Spinal Cord: MRI typically shows lesions in the optic nerves, spinal cord, and sometimes the brain. Lesions are often longitudinally extensive.
3. Clinical Manifestations: Two or more episodes of optic neuritis or transverse myelitis, along with the presence of anti-AQP4 antibodies, confirm the diagnosis.
Step 3: Differential Diagnosis:
1. Multiple Sclerosis (MS): MS also presents with optic neuritis and myelitis, but it typically involves multiple areas of the CNS and does not involve AQP4 antibodies.
2. Systemic Lupus Erythematosus (SLE): SLE can present with neurologic symptoms, but it often involves a more diffuse pattern of CNS involvement.
3. Infections and Vascular Causes: These may mimic NMOSD, especially when there is transverse myelitis or optic neuritis.
Step 4: Management:
1. Acute Attack Treatment: High-dose corticosteroids (e.g., methylprednisolone) are used for acute attacks to reduce inflammation.
2. Plasmapheresis or IVIG: In cases of refractory disease, plasmapheresis or intravenous immunoglobulin (IVIG) may be used.
3. Chronic Management: Long-term immunosuppressive therapy, including azathioprine, mycophenolate mofetil, rituximab, or eculizumab, is used to prevent relapses. Quick Tip: Early diagnosis and prompt treatment of acute attacks are essential to prevent long-term disability in patients with NMOSD.
Discuss the concepts, clinical implications, and the management of nodo-paranodopathies.
View Solution
Nodo-paranodopathies are a group of disorders involving the lymph nodes and adjacent structures, often characterized by their presentation with enlarged lymph nodes and associated clinical features.
Step 1: Concepts of Nodo-Paranodopathies:
1. Definition: Nodo-paranodopathies refer to diseases where both the lymph nodes (nodal involvement) and the surrounding structures (paranodal involvement) are affected, leading to enlargement and possibly inflammation.
2. Etiology: They can arise due to infections, malignancies, autoimmune conditions, or systemic inflammatory diseases.
Step 2: Clinical Implications:
1. Infections: Common infections such as tuberculosis, HIV, or mononucleosis can lead to nodal and paranodal involvement, manifesting as enlarged, tender lymph nodes.
2. Malignancies: Lymphoma, metastasis, or other cancers may present with swollen lymph nodes, and in some cases, paranodal structures like blood vessels or connective tissues may also be involved.
3. Autoimmune Diseases: Conditions like systemic lupus erythematosus (SLE) and rheumatoid arthritis may lead to both nodal and paranodal involvement, contributing to generalized inflammation and lymphadenopathy.
Step 3: Management:
1. Diagnosis: Diagnosis involves clinical evaluation, imaging studies (e.g., ultrasound, CT scans), and biopsy of affected lymph nodes for histopathological analysis.
2. Treatment: Treatment is primarily based on the underlying cause of the nodo-paranodopathy. For infections, antimicrobial therapy is used; for malignancies, chemotherapy or radiation therapy may be required; and for autoimmune diseases, immunosuppressive treatments are employed.
3. Symptomatic Management: Symptomatic treatment for pain and inflammation may include analgesics and corticosteroids.
Step 4: Prognosis:
The prognosis depends on the underlying cause. Infections typically resolve with appropriate treatment, while malignancies and autoimmune diseases may require long-term management and have a variable outlook. Quick Tip: Nodo-paranodopathies are complex disorders requiring a multidisciplinary approach for diagnosis and treatment, with outcomes largely depending on the underlying etiology.
Describe the role of non-invasive neuromodulation in headache disorders.
View Solution
Non-invasive neuromodulation is an emerging therapeutic strategy for treating headache disorders, particularly those that are resistant to traditional pharmacological treatments. This approach involves modulating neural activity through external devices, offering a non-invasive, safe, and often effective alternative.
Step 1: Types of Non-Invasive Neuromodulation Techniques:
1. Transcranial Magnetic Stimulation (TMS): TMS uses magnetic pulses to stimulate specific areas of the brain involved in headache pathophysiology. It is primarily used for treating acute migraine attacks and chronic migraines. TMS can reduce the frequency and severity of migraines by modulating cortical excitability.
2. Transcranial Direct Current Stimulation (tDCS): tDCS involves applying a low electrical current to the scalp, which can alter the excitability of cortical neurons. tDCS has been shown to reduce the frequency of episodic migraines and chronic tension-type headaches.
3. Cervical Spinal Cord Stimulation (SCS): This technique involves applying electrical stimulation to the cervical spine, which may influence the central pain processing pathways involved in headache disorders. It is often used for chronic cluster headaches and refractory migraine cases.
4. Peripheral Nerve Stimulation (PNS): PNS uses electrical pulses to stimulate peripheral nerves such as the occipital nerve, which is often involved in cluster headaches and migraines. This method has been shown to reduce headache frequency and intensity.
Step 2: Mechanisms of Action:
1. Cortical Excitability Modulation: Non-invasive neuromodulation techniques can influence cortical excitability, reducing the likelihood of headache attacks. This is particularly relevant in conditions like migraines, where abnormal cortical activity is believed to play a central role.
2. Pain Pathway Alteration: Techniques like SCS and PNS can alter pain processing at the spinal and peripheral levels, reducing the central sensitization that is often present in chronic headache disorders.
3. Neurochemical Modulation: Non-invasive neuromodulation has the potential to modulate neurotransmitters, such as serotonin and dopamine, which play key roles in headache pathogenesis.
Step 3: Clinical Applications:
1. Acute Migraine Attacks: TMS has been shown to be effective in reducing the severity and duration of acute migraine attacks when applied early in the attack.
2. Chronic Migraine and Tension-Type Headaches: tDCS has demonstrated efficacy in reducing the frequency and severity of chronic migraines and tension-type headaches.
3. Cluster Headaches: Peripheral nerve stimulation, particularly occipital nerve stimulation, has been proven effective for patients with chronic or refractory cluster headaches.
Step 4: Advantages and Limitations:
1. Advantages: Non-invasive neuromodulation techniques are generally well-tolerated, have fewer side effects compared to pharmacological treatments, and offer long-term benefits with ongoing use.
2. Limitations: These techniques are not universally effective for all patients, and results can vary based on the type of headache and the individual’s response. Additionally, devices can be expensive, and some may require ongoing sessions for optimal results. Quick Tip: Non-invasive neuromodulation offers a promising alternative to traditional headache treatments, especially for patients who are not responsive to medication.
List the causes of facial diplegia.
View Solution
Facial diplegia refers to the paralysis of both sides of the face, often resulting from a condition affecting the facial nerve. It can be caused by a variety of neurological, systemic, and infectious conditions. The following are common causes:
Step 1: Neurological Causes:
1. Bilateral Bell's Palsy: An idiopathic, viral infection of the facial nerve that leads to sudden, unilateral or bilateral facial paralysis.
2. Stroke: A bilateral stroke involving the brainstem or higher motor areas can result in facial diplegia.
3. Multiple Sclerosis: MS can cause demyelination of the facial nerve pathways, leading to bilateral facial weakness or paralysis.
4. Guillain-Barré Syndrome: An autoimmune condition that can affect the peripheral nervous system, causing facial diplegia as part of a general weakness pattern.
Step 2: Infectious Causes:
1. Viral Infections: Herpes simplex virus (HSV), varicella-zoster virus (VZV), and Epstein-Barr virus (EBV) can affect the facial nerve, causing bilateral paralysis.
2. Meningitis: Bacterial or viral infections of the meninges can involve the facial nerve, leading to bilateral facial weakness.
Step 3: Systemic Causes:
1. Sarcoidosis: A systemic inflammatory disease that can involve the facial nerve, leading to bilateral facial palsy.
2. Tumors: Tumors of the brainstem or facial nerve can compress both sides of the facial nerve, causing bilateral paralysis. Quick Tip: Facial diplegia often requires a comprehensive neurological evaluation to identify the underlying cause, which may involve imaging, lab tests, and a thorough clinical assessment.
Discuss in detail the approach, diagnosis, and management of facial diplegia.
View Solution
Facial diplegia, characterized by the paralysis of both sides of the face, can result from a variety of conditions. It requires a systematic approach for accurate diagnosis and management.
Step 1: Approach to Diagnosis:
1. Clinical History: A thorough history should be obtained, including the onset, progression, and associated symptoms (e.g., weakness, sensory loss, pain). A history of recent infections, trauma, or systemic diseases should also be considered.
2. Physical Examination: Perform a detailed neurological examination, assessing the motor function of the facial muscles and checking for asymmetry in facial movements. Check for other neurological deficits.
3. Differential Diagnosis: Consider other conditions that can cause bilateral facial weakness, such as strokes, multiple sclerosis, and inflammatory or infectious causes.
Step 2: Diagnostic Tests:
1. MRI or CT Scan: Imaging studies are essential for evaluating structural causes like tumors, strokes, or lesions in the brainstem or facial nerve.
2. Electromyography (EMG): This test can help assess nerve function and differentiate between peripheral and central causes of facial diplegia.
3. Blood Tests: Tests for infections, autoimmune diseases, or metabolic disorders may be indicated.
Step 3: Management:
1. Medical Management:
- Corticosteroids: In cases of Bell’s palsy or inflammatory causes, corticosteroids are often used to reduce inflammation and promote nerve recovery.
- Antiviral Agents: If a viral infection (e.g., herpes simplex or varicella-zoster) is identified, antiviral therapy may be initiated.
- Immunosuppressive Drugs: In cases where facial diplegia is due to an autoimmune disease like sarcoidosis, immunosuppressants may be required.
2. Physical Therapy: Rehabilitation with facial exercises can help improve muscle tone and function. Facial nerve stimulation may also aid recovery.
3. Surgical Intervention: Surgery may be required if facial diplegia is caused by a structural problem, such as a tumor or compression of the facial nerve. In severe or persistent cases, surgical options like nerve grafts or nerve decompression may be considered.
Step 4: Prognosis:
The prognosis of facial diplegia depends on the underlying cause. Recovery is often good in cases of Bell’s palsy, but may be slower or incomplete in cases of stroke, multiple sclerosis, or other systemic conditions. Quick Tip: Prompt diagnosis and targeted treatment are essential for improving the functional outcomes in patients with facial diplegia. Early physical therapy can aid recovery and prevent long-term complications.
Discuss the various presentations, diagnosis and management of spontaneous intracranial hypotension.
View Solution
Step 1: Presentations of Spontaneous Intracranial Hypotension:
Spontaneous intracranial hypotension (SIH) is characterized by low cerebrospinal fluid (CSF) pressure and can present with the following symptoms:
1. Headache: The most common presentation is a positional headache, which worsens when standing and improves when lying down.
2. Nausea and Vomiting: Patients may experience nausea and vomiting associated with the headache.
3. Neck Pain: Some patients present with neck pain or stiffness.
4. Tinnitus: A ringing or buzzing sound in the ears can be a symptom of SIH.
5. Visual Changes: Blurred vision or double vision may also be observed in some patients.
Step 2: Diagnosis of Spontaneous Intracranial Hypotension:
1. MRI of the Brain: The imaging modality of choice is an MRI with gadolinium contrast, which can show features like pachymeningeal enhancement and sagging of the brain.
2. CSF Pressure Measurement: A lumbar puncture may be performed to measure the CSF pressure, which will be low in SIH.
3. CT Myelography: This may be used to identify a CSF leak in the spine, which is the most common cause of SIH.
4. Radioisotope Scanning: In cases where the source of the CSF leak is difficult to locate, a radioisotope scan may be used to identify the leak.
Step 3: Management of Spontaneous Intracranial Hypotension:
1. Conservative Management: Initial management may include bed rest, increased fluid intake, and caffeine to improve CSF pressure.
2. Epidural Blood Patch: If conservative measures fail, an epidural blood patch may be performed, where a small amount of the patient's blood is injected into the epidural space to seal the leak.
3. Surgical Intervention: In cases of persistent leaks, surgery may be required to repair the leak in the spinal cord or dura mater.
4. Medications: Analgesics such as NSAIDs and corticosteroids may be used to manage pain and inflammation associated with SIH. Quick Tip: Prompt diagnosis and appropriate treatment of spontaneous intracranial hypotension can significantly improve symptoms and prevent long-term complications.
Describe the approach to a young patient with extrapyramidal and cognitive dysfunction. [10]
View Solution
The approach to a young patient with both extrapyramidal and cognitive dysfunction involves a comprehensive clinical evaluation, including a detailed history, physical examination, and appropriate diagnostic workup to identify the underlying cause.
Step 1: Clinical History:
1. Onset and Progression: Determine the age of onset, rate of progression, and specific symptoms such as tremors, rigidity, bradykinesia, or cognitive impairment.
2. Family History: Investigate a family history of neurodegenerative disorders, metabolic conditions, or movement disorders, as genetic causes may be involved.
3. Exposure History: Assess exposure to toxins, medications (such as antipsychotics), or infections that might lead to extrapyramidal symptoms or cognitive dysfunction.
Step 2: Physical Examination:
1. Neurological Examination: A thorough neurological exam should include assessment of motor function (muscle tone, coordination, reflexes) and cognitive function (memory, attention, language, executive function).
2. Movement Disorders: Evaluate for features of Parkinsonism, dystonia, chorea, or tremor, which may suggest a diagnosis of a movement disorder such as Wilson’s disease or Huntington’s disease.
3. Cognitive Testing: Perform basic cognitive testing such as the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) to assess memory, attention, and other cognitive functions.
Step 3: Diagnostic Workup:
1. Laboratory Tests: Basic metabolic panels, liver function tests, and thyroid function tests should be done to rule out metabolic and endocrine causes.
2. Genetic Testing: If hereditary disorders like Huntington’s disease or Wilson’s disease are suspected, genetic testing should be considered.
3. Imaging Studies: Brain imaging (MRI or CT) may reveal structural abnormalities such as atrophy or lesions that could suggest neurodegenerative diseases.
4. Neurophysiological Studies: Electromyography (EMG) and nerve conduction studies may be useful in diagnosing conditions affecting the peripheral nervous system.
Step 4: Management:
1. Symptomatic Treatment: Management depends on the underlying diagnosis. For extrapyramidal symptoms, medications like levodopa, dopamine agonists, or anticholinergics may be used. Cognitive dysfunction can be managed with cognitive therapy or medications targeting the specific etiology.
2. Multidisciplinary Approach: A team of neurologists, physiotherapists, and psychologists may be needed for optimal management, especially for neurodegenerative diseases.
3. Genetic Counseling: For genetic conditions, provide genetic counseling and consider screening family members. Quick Tip: A detailed history and thorough neurological examination are key to distinguishing between different movement disorders and cognitive impairments in young patients.
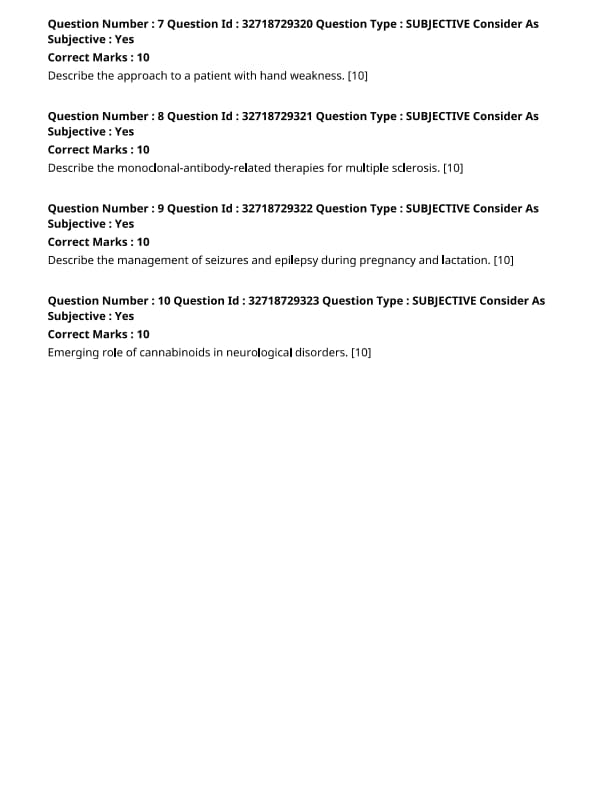
Describe the approach to a patient with hand weakness.
View Solution
Hand weakness can result from a variety of neurological, muscular, or systemic conditions. A thorough approach involves a detailed history, clinical examination, and appropriate diagnostic tests.
Step 1: History Taking:
1. Onset and Duration: Determine whether the weakness is acute or chronic. Acute weakness may suggest a neurological event like stroke or Guillain-Barré syndrome, whereas chronic weakness may point to conditions like muscular dystrophy or peripheral neuropathy.
2. Associated Symptoms: Inquire about any sensory changes, pain, numbness, or loss of coordination. Associated symptoms can help localize the lesion.
3. Medical History: Ask about diabetes, autoimmune diseases, or previous trauma that may predispose the patient to conditions like carpal tunnel syndrome or peripheral neuropathy.
Step 2: Clinical Examination:
1. Inspection: Look for signs of muscle wasting, deformities, or asymmetry in the hands.
2. Palpation: Palpate the muscles to assess for tenderness, spasm, or hypertrophy.
3. Motor Testing: Test muscle strength using the Medical Research Council (MRC) scale. Assess for weakness in specific muscle groups (e.g., flexors, extensors) and hand grip strength.
4. Sensory Examination: Check for any loss of sensation or abnormal sensations like tingling or burning.
5. Reflexes: Assess deep tendon reflexes (e.g., biceps, triceps, brachioradialis) to identify possible involvement of the central nervous system.
Step 3: Differential Diagnosis:
1. Neurological Causes: Conditions like stroke, cervical radiculopathy, carpal tunnel syndrome, multiple sclerosis, or amyotrophic lateral sclerosis (ALS) can present with hand weakness.
2. Muscular Causes: Muscular dystrophies, polymyositis, or muscular atrophy may present with progressive weakness.
3. Systemic Conditions: Conditions like diabetes (diabetic neuropathy), hypothyroidism, or vitamin deficiencies (e.g., B12) can also cause hand weakness.
Step 4: Diagnostic Tests:
1. Blood Tests: Complete blood count, electrolytes, thyroid function tests, vitamin levels, and autoimmune markers can help identify systemic causes.
2. Electromyography (EMG) and Nerve Conduction Studies: These are crucial to evaluate the function of muscles and peripheral nerves.
3. Imaging: MRI of the brain and cervical spine may be indicated if central nervous system involvement is suspected.
4. Genetic Testing: For suspected inherited muscular disorders, genetic testing may be warranted.
Step 5: Management:
1. Treatment of Underlying Condition: Based on the diagnosis, treat the underlying cause (e.g., steroids for inflammatory conditions, surgical decompression for carpal tunnel syndrome).
2. Physical Therapy: Rehabilitation, including strengthening exercises and occupational therapy, may be required for improving hand function.
3. Symptom Control: Analgesics, corticosteroids, or immunosuppressants may be prescribed for managing inflammation or neuropathic pain. Quick Tip: A thorough clinical examination and targeted diagnostic tests are crucial to identify the cause of hand weakness and guide appropriate treatment.
Describe the monoclonal-antibody-related therapies for multiple sclerosis.
View Solution
Monoclonal antibody therapies are an important class of treatments for multiple sclerosis (MS), particularly for patients with relapsing forms of the disease. These therapies target specific immune system components involved in the pathogenesis of MS, aiming to reduce inflammation, prevent relapses, and slow disease progression.
Step 1: Mechanism of Action of Monoclonal Antibodies in MS:
Monoclonal antibodies work by targeting specific immune cells or molecules involved in the autoimmune attack that damages the central nervous system (CNS) in MS. The main target of these therapies is the immune cells, specifically the B-cells, T-cells, and the molecules that mediate immune responses.
1. B-cell depletion: B-cells play a critical role in MS by producing antibodies that target the myelin sheath. Monoclonal antibodies such as rituximab and ocrelizumab deplete B-cells, thereby reducing inflammation and preventing the activation of T-cells that damage the myelin.
2. T-cell modulation: Some monoclonal antibodies target specific T-cells or molecules that regulate the immune response, such as natalizumab, which prevents T-cells from entering the CNS, thereby reducing inflammation and damage to myelin.
Step 2: Examples of Monoclonal Antibodies Used in MS Treatment:
1. Ocrelizumab (Ocrevus): Ocrelizumab is a monoclonal antibody that targets CD20 on B-cells, leading to their depletion. It is used for the treatment of both relapsing and primary progressive forms of MS. It has been shown to reduce relapse rates and slow disease progression.
2. Rituximab (Rituxan): Rituximab is also a CD20-targeting monoclonal antibody that is used off-label in MS treatment. Like ocrelizumab, it depletes B-cells and has demonstrated efficacy in reducing relapses and preventing disease progression.
3. Natalizumab (Tysabri): Natalizumab is an integrin inhibitor that prevents T-cells from migrating into the CNS. It is highly effective in reducing relapses and is used in patients with aggressive MS or those who are unresponsive to other treatments.
4. Alemtuzumab (Lemtrada): Alemtuzumab targets CD52, a protein found on the surface of B-cells, T-cells, and other immune cells. It induces depletion of these cells and has shown significant efficacy in relapsing forms of MS.
Step 3: Benefits and Side Effects of Monoclonal Antibodies:
1. Benefits: Monoclonal antibodies offer a targeted approach to MS treatment with proven efficacy in reducing relapses, slowing disability progression, and reducing the frequency of MRI-detected lesions. These therapies are often used in patients with more severe or treatment-resistant MS.
2. Side Effects: While monoclonal antibodies are effective, they can have side effects, including infusion reactions, infections (due to immune system modulation), and, in some cases, a higher risk of malignancies. Monitoring during treatment is essential to minimize these risks.
Step 4: Considerations in Treatment Selection:
1. Disease Type: The choice of monoclonal antibody may depend on the type of MS (relapsing or progressive) and the severity of the disease.
2. Patient's Health Status: Factors such as comorbidities, prior treatment responses, and the patient's immune status must be considered when selecting the appropriate therapy.
3. Safety Profile: Due to the potential side effects, it is crucial to consider the patient's risk factors for infections, malignancies, and other complications when initiating monoclonal antibody therapy. Quick Tip: Monoclonal antibody therapies offer significant benefits in managing relapsing MS, but careful patient selection and monitoring are essential due to potential side effects.
Describe the management of seizures and epilepsy during pregnancy and lactation.
View Solution
Managing seizures and epilepsy during pregnancy and lactation presents a unique challenge as it involves balancing the health of the mother, fetus, and infant. It is essential to carefully select anticonvulsant therapy to minimize risks to both mother and child.
Step 1: General Principles:
1. Preconception Counseling: Women with epilepsy should have a discussion with their healthcare provider before conception to optimize the management of their condition and minimize risks to the pregnancy. This includes assessing seizure control and potential teratogenic effects of medications.
2. Goal of Treatment: The goal is to achieve seizure control with the lowest possible dose of medication to minimize fetal and maternal risks. Seizures during pregnancy can lead to maternal injury, fetal hypoxia, or preterm labor.
Step 2: Pharmacologic Management During Pregnancy:
1. Antiepileptic Drugs (AEDs): Commonly used AEDs include:
- Levetiracetam: Considered the first-line choice due to its safety profile and low risk of teratogenicity.
- Lamotrigine: Another safe option with minimal fetal risks, often preferred in women with generalized epilepsy.
- Carbamazepine: Can be used but carries a risk of neural tube defects, so folic acid supplementation is strongly recommended.
- Valproate: Should be avoided due to its high teratogenic risk, including an increased risk of neural tube defects and developmental delay.
2. Folic Acid Supplementation: High-dose folic acid (4-5 mg/day) should be started prior to conception to reduce the risk of neural tube defects, especially for women on AEDs like carbamazepine or valproate.
3. Monitor Plasma Drug Levels: Since pregnancy can affect drug metabolism, monitoring plasma drug levels is necessary to ensure therapeutic efficacy and avoid toxicity.
Step 3: Non-Pharmacologic Management:
1. Lifestyle Modifications: Adequate sleep, stress management, and avoiding triggers (e.g., flashing lights, lack of sleep) are essential components of seizure control.
2. Diet and Exercise: A balanced diet and regular exercise, under medical supervision, can improve overall health and well-being during pregnancy.
Step 4: Management During Labor and Delivery:
1. Seizure Prophylaxis: Continue AED therapy during labor to prevent breakthrough seizures.
2. Monitoring: Continuous fetal and maternal monitoring is essential to detect any signs of distress during labor.
3. Emergency Seizure Management: If seizures occur during labor, intravenous lorazepam or diazepam can be used to control seizures.
4. Cesarean Section: A cesarean delivery may be indicated in the case of severe uncontrolled seizures, but vaginal delivery is generally safe for well-controlled patients.
Step 5: Management During Lactation:
1. Breastfeeding Considerations: Most AEDs are excreted in breast milk, but the levels are generally low and not harmful to the infant.
- Levetiracetam and Lamotrigine: Both are considered safe for breastfeeding.
- Carbamazepine and Phenytoin: These drugs are also compatible with breastfeeding, but their levels should be monitored.
- Valproate: Should be avoided during lactation due to the risk of adverse effects on the infant.
2. Monitor Infant: Monitor the infant for signs of sedation or feeding difficulties, especially in the first few weeks of life.
Step 6: Postpartum Care:
1. AED Dosage Adjustment: After delivery, the medication dosage may need to be adjusted, as drug metabolism can change postpartum.
2. Postpartum Seizures: Seizures can occur in the postpartum period due to hormonal changes, stress, or inadequate medication levels. Ensure adequate follow-up with regular neurologic assessments. Quick Tip: The management of epilepsy during pregnancy and lactation requires careful consideration of the risks of seizures, the potential teratogenic effects of AEDs, and the safety of both the mother and the child.
Emerging role of cannabinoids in neurological disorders.
View Solution
Step 1: Overview of Cannabinoids:
Cannabinoids are a group of chemical compounds found in cannabis that have the ability to act on the body’s cannabinoid receptors. These receptors are part of the endocannabinoid system, which is involved in various physiological processes, including mood, memory, and pain sensation. The most commonly studied cannabinoids are tetrahydrocannabinol (THC) and cannabidiol (CBD).
Step 2: Role in Neurological Disorders:
1. Epilepsy: Cannabinoids, particularly CBD, have shown promise in the treatment of drug-resistant epilepsy, especially in children with conditions like Dravet syndrome and Lennox-Gastaut syndrome. Studies have demonstrated that CBD can reduce the frequency and severity of seizures.
2. Multiple Sclerosis (MS): In MS, cannabinoids have been found to help reduce spasticity, pain, and improve sleep quality. Both THC and CBD are being investigated for their potential benefits in managing MS symptoms.
3. Parkinson's Disease: Cannabinoids have been explored for their ability to reduce tremors and improve motor function in patients with Parkinson's disease. Some studies suggest that cannabinoids might help alleviate motor symptoms and improve the quality of life.
4. Alzheimer's Disease: Preliminary research suggests that cannabinoids could have neuroprotective effects in Alzheimer’s disease by reducing inflammation and oxidative stress, potentially slowing disease progression.
5. Neuropathic Pain: Cannabinoids have been shown to have analgesic effects and are often used in the management of neuropathic pain, providing relief for patients with conditions such as diabetic neuropathy and fibromyalgia.
Step 3: Mechanism of Action:
Cannabinoids exert their effects by binding to cannabinoid receptors (CB1 and CB2) in the brain and nervous system. These interactions influence neurotransmitter release, modulate inflammation, and protect neurons from damage.
Step 4: Challenges and Considerations:
1. Legal and Ethical Issues: The legal status of cannabinoids varies by country and state, limiting their widespread clinical use. Further regulation and standardization are needed.
2. Side Effects: While cannabinoids are generally well-tolerated, they can cause side effects such as dizziness, drowsiness, and cognitive impairment, particularly with THC.
3. Long-Term Effects: The long-term effects of cannabinoid use, particularly for neurological disorders, are still under investigation. More robust clinical trials are required to fully understand the safety and efficacy. Quick Tip: Cannabinoids have shown potential in managing neurological disorders, but further research is necessary to establish their long-term safety and effectiveness.




Comments