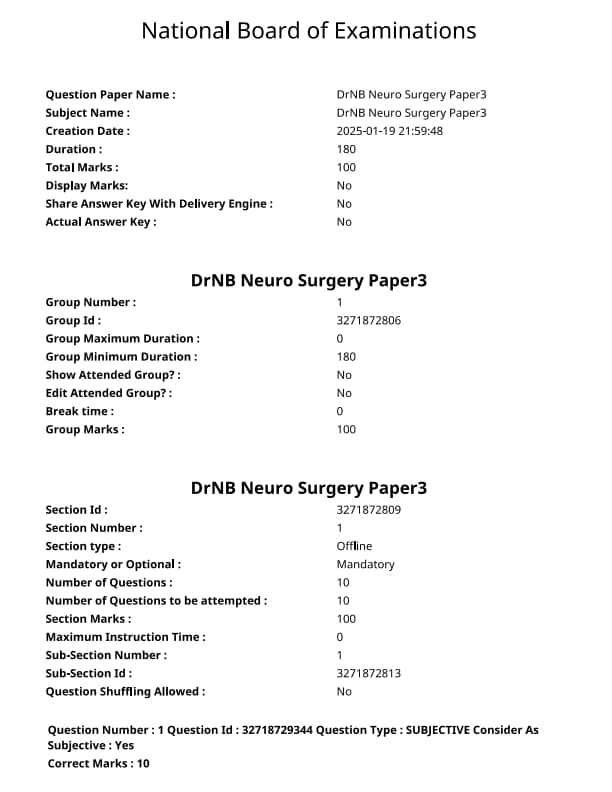
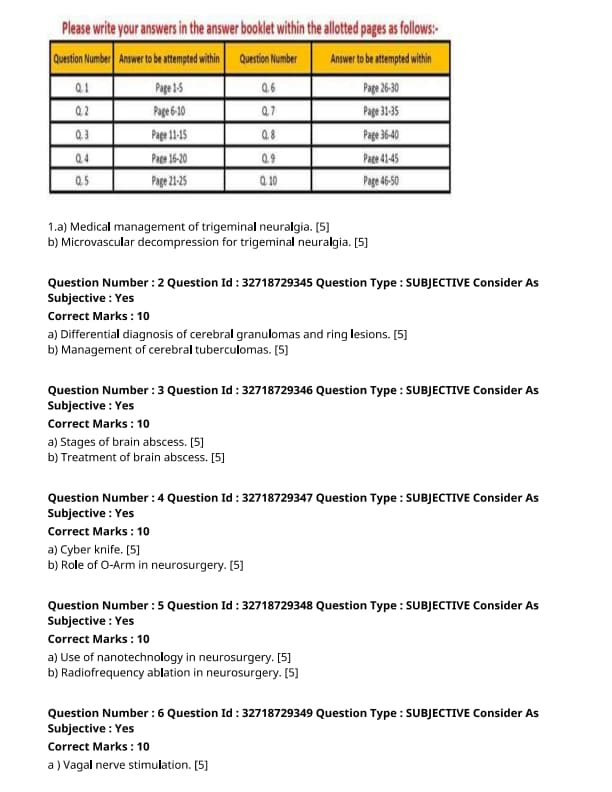
NEET SS 2024 DrNB Neuro Surgery Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Neuro Surgery Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Neuro Surgery Paper 3 Question Paper | Check Solutions |

Medical management of trigeminal neuralgia.
View Solution
Trigeminal neuralgia is characterized by sudden, severe, stabbing pain along the trigeminal nerve distribution. Medical management primarily involves the use of anticonvulsants and other medications to manage the pain.
Step 1: First-line Medications:
1. Carbamazepine: This is the most commonly used drug for trigeminal neuralgia. It works by inhibiting the sodium channels in neurons and reducing nerve excitability.
2. Oxcarbazepine: An alternative to carbamazepine, it has a similar mechanism of action and fewer side effects.
Step 2: Second-line Medications:
1. Gabapentin or Pregabalin: These drugs, which are GABA analogs, can be effective for pain relief in cases where carbamazepine is not well tolerated or ineffective.
2. Baclofen: A muscle relaxant that can help reduce pain by inhibiting the release of excitatory neurotransmitters at the synaptic level.
Step 3: Adjunctive Therapies:
1. Tricyclic Antidepressants (TCAs): Medications like amitriptyline may be used in cases where pain is more persistent.
2. Topical Lidocaine: In some patients, a topical anesthetic applied to the affected area may provide temporary relief. Quick Tip: If medical management is ineffective, surgical options such as microvascular decompression may be considered for long-term relief.
Microvascular decompression for trigeminal neuralgia.
View Solution
Microvascular decompression (MVD) is a surgical procedure used to treat trigeminal neuralgia, particularly in patients who do not respond to medical management or in those who experience significant side effects from medications.
Step 1: Surgical Technique:
1. Accessing the Trigeminal Nerve: The surgery is performed via a craniotomy, where a small opening is made in the skull near the cerebellum to access the trigeminal nerve root.
2. Decompression: The surgeon identifies the blood vessels compressing the trigeminal nerve and separates them from the nerve using Teflon pledgets or other materials to relieve the pressure.
Step 2: Indications for MVD:
1. Failure of Medical Management: When anticonvulsants and other drugs fail to adequately control the pain or cause intolerable side effects.
2. Good Surgical Candidates: MVD is often more effective in patients with typical trigeminal neuralgia caused by vascular compression, especially those who are relatively young and healthy.
Step 3: Postoperative Care and Outcomes:
1. Recovery Time: Most patients can return to normal activities within a few weeks, but pain relief may take time.
2. Complications: Potential risks include facial weakness, hearing loss, cerebrospinal fluid leaks, or recurrence of neuralgia. Quick Tip: Microvascular decompression offers long-term pain relief and is the most effective surgical option for trigeminal neuralgia when medical therapy fails.
Differential diagnosis of cerebral granulomas and ring lesions.
View Solution
Cerebral granulomas and ring lesions are often seen on imaging studies such as CT or MRI. They can be caused by a variety of conditions, and differentiating them is essential for appropriate management.
Step 1: Causes of Cerebral Granulomas and Ring Lesions:
1. Infectious Etiologies:
- Tuberculosis (TB): Cerebral tuberculomas present as ring-enhancing lesions, typically in immunocompromised individuals or endemic areas.
- Fungal Infections: Fungal infections such as cryptococcosis and histoplasmosis can also cause granulomas and ring lesions.
- Parasitic Infections: Neurocysticercosis, caused by the pork tapeworm, commonly presents as cystic lesions with ring enhancement.
- Bacterial Infections: Brain abscesses due to bacterial infections can present as ring-enhancing lesions, often with associated mass effect.
2. Non-Infectious Causes:
- Sarcoidosis: Granulomas in the brain may occur due to systemic sarcoidosis, with or without involvement of other organs.
- Multiple Sclerosis (MS): In MS, ring-enhancing lesions may occur in the periventricular region, often associated with demyelination.
- Neoplastic Conditions: Metastatic brain tumors can cause ring-enhancing lesions, especially from primary cancers like lung, breast, or colon.
- Granulomatosis with Polyangiitis (Wegener’s Granulomatosis): This autoimmune condition can lead to granulomatous lesions in the central nervous system.
Step 2: Imaging Findings:
1. CT/MRI: Ring-enhancing lesions are seen with contrast on CT or MRI scans. The enhancement is often indicative of a breakdown in the blood-brain barrier, as seen in abscesses, tumors, or granulomas.
2. Biopsy or Culture: In cases where the diagnosis is unclear, a biopsy or culture of the lesion may be required to identify the causative organism or confirm the presence of granulomatous tissue. Quick Tip: Ring-enhancing lesions can result from a variety of conditions, including infections, autoimmune diseases, and neoplasms, so a thorough diagnostic work-up is essential.
Management of cerebral tuberculomas.
View Solution
Cerebral tuberculomas are localized collections of tuberculosis infection in the brain, often presenting with neurological symptoms due to mass effect or inflammatory responses.
Step 1: Medical Management:
1. Antituberculous Therapy (ATT):
- First-line treatment involves a combination of antituberculous drugs, typically isoniazid, rifampicin, pyrazinamide, and ethambutol for a minimum of 6 to 12 months.
- Directly Observed Therapy (DOT) may be used to ensure adherence to the treatment regimen.
- ATT should be started as soon as the diagnosis is suspected, even before culture results are available, to reduce the risk of further progression and complications.
2. Corticosteroids:
- Corticosteroids, such as prednisone, are commonly used to reduce inflammation and mass effect caused by the tuberculomas. This helps in minimizing neurological damage and controlling symptoms like headaches and seizures.
Step 2: Surgical Management:
1. Surgical Resection:
- If the tuberculomas cause significant mass effect, seizures, or are unresponsive to medical therapy, surgical resection may be considered.
- Surgery is also indicated in cases of abscess formation or if there is suspicion of malignancy.
Step 3: Follow-up and Monitoring:
1. Regular Imaging:
- MRI or CT scans are performed periodically to monitor the response to treatment and detect any recurrence of tuberculomas.
- Follow-up with regular neurological exams to assess improvement or development of new neurological deficits.
2. Adherence to Therapy:
- It is crucial to ensure that the patient completes the full course of ATT to prevent relapse or development of drug-resistant tuberculosis. Quick Tip: Early diagnosis and prompt treatment with antituberculous drugs and steroids are essential to prevent complications and improve outcomes in cerebral tuberculomas.
Stages of brain abscess.
View Solution
Brain abscesses are localized infections within the brain tissue, often resulting from bacterial, fungal, or parasitic infections. The abscess develops in stages, with distinct phases of progression.
Step 1: Stages of Brain Abscess Formation:
1. Early Stage (Inflammatory Stage): This stage typically occurs within the first few days to weeks after infection. In this phase, a localized inflammatory response occurs at the site of infection, leading to edema (swelling) and the formation of a small collection of pus. The surrounding tissue may become necrotic.
2. Suppurative Stage (Pus Formation): As the infection progresses, the body responds by increasing the production of pus, which accumulates at the center of the abscess. This stage involves the formation of a thick, encapsulated collection of pus surrounded by inflammatory cells.
3. Mature Stage (Encapsulation): Over time, the abscess becomes encapsulated by a fibrous membrane. This barrier helps to limit the spread of infection, but the abscess continues to exert pressure on surrounding brain tissue. The center of the abscess remains filled with pus, which may be composed of dead tissue, bacteria, and inflammatory cells.
4. Resolution or Complication Stage: If untreated, the abscess may continue to grow, leading to increased intracranial pressure, and may cause permanent brain damage. In some cases, the abscess may resolve on its own or with treatment, but complications such as brain herniation or rupture into the ventricular system can occur. Quick Tip: Brain abscesses progress through distinct stages, and timely diagnosis and treatment are crucial to preventing complications.
Treatment of brain abscess.
View Solution
The treatment of a brain abscess involves a combination of medical and surgical interventions. The aim is to eradicate the infection, reduce intracranial pressure, and prevent further neurological damage.
Step 1: Medical Treatment:
1. Antibiotics: The first step in treating a brain abscess is the use of intravenous antibiotics to target the causative organisms. Broad-spectrum antibiotics are typically started initially, followed by more targeted therapy once the specific microorganism is identified. The treatment course may last for several weeks.
2. Antifungal or Antiparasitic Therapy: If the abscess is caused by fungi or parasites, specific antifungal or antiparasitic medications are prescribed. For example, in cases of fungal abscesses, drugs like amphotericin B may be used.
3. Steroids: Corticosteroids such as dexamethasone may be administered to reduce inflammation and edema surrounding the abscess, thus decreasing intracranial pressure.
4. Seizure Prophylaxis: Anticonvulsants may be used to prevent seizures, which are a common complication of brain abscesses.
Step 2: Surgical Treatment:
1. Abscess Drainage: If the abscess is large, or if the patient is not responding to medical treatment, surgical drainage may be required. This involves either aspiration of the pus using a needle or, in some cases, surgical resection of the abscess.
2. Craniotomy: In severe cases, a craniotomy may be performed to remove the abscess and reduce the pressure on the brain.
3. Monitoring: Post-surgical monitoring of intracranial pressure, neurological status, and infection markers is essential to prevent complications and ensure proper recovery.
Step 3: Post-treatment Care:
1. Rehabilitation: After the abscess is treated, patients may require rehabilitation to recover lost neurological function. This can include physical, occupational, and speech therapy.
2. Long-term Follow-up: Ongoing follow-up is necessary to ensure there is no recurrence of the infection and to manage any long-term neurological deficits. Quick Tip: Early diagnosis and a combination of antibiotic therapy and surgical drainage are key to effective treatment of brain abscesses.
Cyber knife.
View Solution
CyberKnife is a non-invasive robotic radiosurgery system used for treating tumors and other medical conditions. It is particularly effective for treating tumors that are difficult to reach with traditional surgery or radiation therapy.
Step 1: Technology Overview:
CyberKnife combines precise robotic technology with advanced imaging systems, allowing for high-dose radiation to be delivered to tumors with great accuracy while minimizing damage to surrounding healthy tissue. It is used in both brain and spine surgery, as well as for tumors in other parts of the body.
Step 2: Applications:
1. Tumor Treatment: CyberKnife is used to treat various types of tumors, including brain, lung, liver, prostate, and pancreatic tumors. It is particularly useful for tumors that are inoperable or located in hard-to-reach areas.
2. Functional Neurosurgery: It can also be used to treat functional disorders like trigeminal neuralgia and certain types of epilepsy, where traditional surgery might carry high risks.
Step 3: Advantages:
1. Non-Invasive: CyberKnife treatment is non-invasive and requires no surgical incision, reducing recovery time and complication risks.
2. Precision: The robot’s precision allows for high-dose radiation delivery directly to the tumor while sparing surrounding healthy tissues.
3. Flexibility: It allows for treatment of tumors from multiple angles without the need for patient repositioning.
Step 4: Limitations:
1. Size of Tumor: It may not be suitable for tumors that are too large or involve critical structures that cannot be spared.
2. Multiple Sessions: Some treatments may require multiple sessions to effectively treat the tumor. Quick Tip: CyberKnife is a cutting-edge technology for treating tumors non-invasively, offering excellent precision and fewer side effects compared to traditional surgical methods.
Role of O-Arm in neurosurgery.
View Solution
The O-Arm is a mobile surgical imaging system used in neurosurgery and other surgical specialties. It provides real-time, high-resolution imaging during surgeries, allowing surgeons to navigate and perform procedures with greater precision.
Step 1: Technology Overview:
The O-Arm uses a combination of X-ray imaging and advanced computer software to produce 3D images of the surgical site. These images can be used for navigation and planning during spinal, brain, and orthopedic surgeries.
Step 2: Applications in Neurosurgery:
1. Spinal Surgery: The O-Arm is commonly used in spinal surgery to provide real-time imaging for spinal alignment, screw placement, and overall procedural guidance. It enhances the accuracy of complex spinal surgeries.
2. Brain Surgery: The O-Arm is also used in brain surgery to provide detailed 3D images of the brain, allowing for precise removal of tumors or other abnormal tissue.
3. Minimally Invasive Procedures: The system is often used for minimally invasive surgeries, where small incisions and precise navigation are critical for reducing patient recovery time.
Step 3: Advantages:
1. Real-Time Imaging: Surgeons can view high-quality images immediately, which helps in adjusting the surgical plan and improving the accuracy of the procedure.
2. Reduced Risk of Complications: By providing detailed anatomical views, the O-Arm helps minimize the risk of complications during surgery.
3. Minimally Invasive: The use of the O-Arm allows for less invasive techniques, reducing trauma to surrounding tissues and improving recovery times.
Step 4: Limitations:
1. Exposure to Radiation: As with any X-ray imaging system, there is a small risk associated with radiation exposure, though it is minimized with the O-Arm’s advanced technology.
2. Cost: The O-Arm system can be expensive, limiting its availability in some healthcare settings. Quick Tip: The O-Arm is a valuable tool in neurosurgery for improving surgical precision, reducing patient risk, and enhancing recovery through real-time, high-resolution imaging.
Use of nanotechnology in neurosurgery.
View Solution
Step 1: Understanding Nanotechnology in Neurosurgery:
Nanotechnology refers to the manipulation and engineering of materials at the nanoscale (typically 1-100 nm). In neurosurgery, it has the potential to revolutionize diagnosis, treatment, and recovery processes.
Step 2: Applications of Nanotechnology in Neurosurgery:
1. Nanoparticles for Drug Delivery: Nanoparticles can be engineered to deliver drugs directly to the brain or to a specific site, improving the effectiveness and reducing systemic side effects. This can be particularly useful in treating brain tumors and neurological disorders.
2. Nanorobots for Surgery: Nanorobots could be used to perform precise surgeries at the cellular level, such as removing tumors or repairing damaged tissues, with minimal invasiveness.
3. Imaging and Diagnostics: Nanoscale materials are being used to enhance brain imaging techniques like MRI, allowing for better detection of abnormalities such as tumors or vascular malformations.
4. Neuroprotective Nanomaterials: Nanomaterials may help protect neurons from damage during trauma or surgery, improving recovery and minimizing neuronal loss.
Step 3: Challenges and Future Directions:
1. Safety and Toxicity: One of the main concerns with the use of nanoparticles in neurosurgery is their potential toxicity. Long-term effects need to be carefully studied.
2. Regulatory Issues: The regulatory approval process for nanotechnology-based treatments is still evolving, which may slow down their clinical application.
3. Cost and Accessibility: As with many cutting-edge technologies, the high cost of nanotechnology may limit its widespread use in clinical practice. Quick Tip: Nanotechnology holds significant promise for revolutionizing neurosurgery, but safety, regulatory, and cost-related challenges remain to be addressed.
Radiofrequency ablation in neurosurgery.
View Solution
Step 1: Understanding Radiofrequency Ablation (RFA) in Neurosurgery:
Radiofrequency ablation (RFA) is a minimally invasive technique that uses high-frequency electrical currents to generate heat, which is used to destroy abnormal tissues, such as tumors or nerve tissues. It is commonly used in various types of surgery, including neurosurgery.
Step 2: Applications of RFA in Neurosurgery:
1. Tumor Treatment: RFA is used to treat certain types of brain and spinal tumors by destroying cancer cells. This can help reduce the size of tumors and relieve symptoms such as pressure or pain.
2. Pain Management: RFA is used to treat chronic pain, particularly in conditions like trigeminal neuralgia and facet joint pain, by targeting and disrupting the nerve pathways transmitting pain signals.
3. Epilepsy Treatment: In patients with drug-resistant epilepsy, RFA can be used to target and ablate areas of the brain that are responsible for initiating seizures, providing relief for some patients.
4. Spinal Disorders: RFA is used in spinal surgery to treat conditions such as herniated discs and spinal stenosis by targeting specific nerve roots responsible for pain.
Step 3: Benefits and Risks of RFA in Neurosurgery:
1. Benefits: RFA is minimally invasive, involves less recovery time, and carries a lower risk of complications compared to traditional surgery.
2. Risks: While generally safe, RFA can lead to potential complications such as infection, bleeding, or damage to adjacent structures, especially in the brain and spinal cord. Quick Tip: Radiofrequency ablation is an effective tool for managing various neurological conditions, but proper patient selection and technique are crucial for minimizing risks.
Vagal nerve stimulation. [5]
View Solution
Vagal nerve stimulation (VNS) is a therapeutic option for patients with epilepsy who do not respond to medical management.
Step 1: Mechanism of Action:
VNS involves the implantation of a small device under the skin in the chest, which sends electrical impulses to the vagus nerve. These electrical impulses modulate the brain’s electrical activity, potentially reducing the frequency and severity of seizures.
Step 2: Indications:
1. Refractory Epilepsy: VNS is primarily used for patients with focal or generalized epilepsy who have not responded to antiepileptic drugs.
2. Patients Who Are Not Surgical Candidates: VNS can be an option for patients who are not candidates for surgical resection due to the location of the seizure focus or other contraindications.
Step 3: Procedure and Follow-up:
1. Implantation: The procedure involves placing an electrode around the left vagus nerve, which is connected to a pulse generator implanted in the chest.
2. Settings and Adjustment: The device is programmed to deliver electrical impulses at regular intervals, and settings may be adjusted periodically to optimize seizure control. Quick Tip: VNS can significantly reduce the frequency of seizures, though it may not eliminate them entirely. Regular follow-up is necessary to adjust settings and monitor effectiveness.
Types of epilepsy surgery. [5]
View Solution
Epilepsy surgery is considered for patients with drug-resistant epilepsy when seizures cannot be controlled with medications. Several types of surgical options are available.
Step 1: Resective Surgery:
1. Focal Cortical Resection: In this procedure, the area of the brain responsible for seizures (the epileptogenic zone) is surgically removed. This is typically performed in patients with a single, well-localized focus of seizures.
2. Hemispherectomy: In cases of severe, widespread epilepsy that affects one hemisphere of the brain, hemispherectomy involves the removal of part or all of one hemisphere to stop seizures.
Step 2: Disconnective Surgery:
1. Corpus Callosotomy: This procedure involves cutting the corpus callosum, which connects the two hemispheres of the brain, in order to limit the spread of seizure activity. This is often performed in patients with generalized seizures.
2. Multiple Subpial Transection: This technique involves making small cuts in the brain tissue to interrupt the spread of seizure activity without removing brain tissue.
Step 3: Laser Ablation:
1. Laser Interstitial Thermal Therapy (LITT): This minimally invasive technique uses a laser to ablate the seizure focus through a small incision. It is used in cases where resection is not feasible. Quick Tip: Epilepsy surgery can offer significant seizure relief in carefully selected patients. It is typically considered after a thorough evaluation of the seizure focus and failure of drug therapy.
Magnetic resonance spectroscopy.
View Solution
Magnetic Resonance Spectroscopy (MRS) is a non-invasive imaging technique that provides biochemical information about tissues, particularly the brain. It measures the concentration of metabolites and helps in diagnosing and monitoring various neurological disorders.
Step 1: Principles of MRS:
1. Metabolite Detection: MRS detects the presence and concentration of various metabolites, such as N-acetylaspartate (NAA), choline, creatine, and lactate, which are important for brain metabolism.
2. Non-Invasive Technique: Unlike biopsy, MRS does not require tissue removal and can be performed alongside conventional MRI scans.
Step 2: Clinical Applications:
1. Brain Tumors: MRS is used to distinguish between malignant and benign tumors, as tumors often show altered metabolite levels.
2. Epilepsy: MRS can identify abnormal metabolic activity in the brain, helping in the localization of epileptic foci.
3. Neurodegenerative Diseases: It is helpful in assessing metabolic changes in diseases such as Alzheimer's disease, multiple sclerosis, and Huntington’s disease.
4. Stroke: MRS can detect ischemic changes in brain tissues and monitor the recovery process.
Step 3: Limitations of MRS:
1. Resolution: MRS typically has lower spatial resolution compared to conventional MRI, limiting its ability to accurately assess small lesions.
2. Technical Challenges: The technique requires specialized equipment and expertise to interpret results. Quick Tip: MRS is an excellent tool for assessing brain metabolism, offering valuable insights in conditions like brain tumors and neurodegenerative diseases.
Magnetic resonance tractography.
View Solution
Magnetic Resonance Tractography (MRT) is a specialized MRI technique used to visualize the white matter tracts in the brain. It is based on the diffusion of water molecules in the brain, particularly along the direction of the fibers.
Step 1: Principles of MRT:
1. Diffusion Tensor Imaging (DTI): MRT is based on DTI, which measures the diffusion of water molecules along the axonal fibers in the white matter. The technique highlights the orientation and integrity of these fibers.
2. Fiber Tracking: MRT maps out the trajectories of white matter fibers, helping to visualize neural connections and brain networks.
Step 2: Clinical Applications:
1. Pre-Surgical Planning: MRT is used to plan surgeries for brain tumors or epilepsy, helping to avoid important fiber tracts and reduce postoperative deficits.
2. Stroke Rehabilitation: MRT is helpful in assessing the extent of damage to white matter after a stroke and guiding rehabilitation strategies.
3. Neurodegenerative Diseases: It helps in monitoring the progression of diseases such as Alzheimer's, where there is disruption in white matter integrity.
4. Multiple Sclerosis: MRT can assess the damage to white matter in patients with MS, aiding in diagnosis and monitoring progression.
Step 3: Limitations of MRT:
1. Resolution: MRT has lower resolution for visualizing small or subtle changes in white matter tracts.
2. Technical Complexity: The technique requires sophisticated software and advanced technical expertise to interpret the images. Quick Tip: Magnetic resonance tractography is a valuable tool for visualizing white matter pathways and aiding in surgical planning and monitoring brain diseases.
Flow diverters.
View Solution
Flow diverters are a type of endovascular device used in the treatment of complex intracranial aneurysms. They work by redirecting blood flow away from the aneurysm, allowing the vessel to remodel and reducing the pressure inside the aneurysm.
Step 1: Mechanism of Action:
1. Stent-like Structure: Flow diverters are essentially stent-like structures that are deployed within the parent artery of the aneurysm. They cover the neck of the aneurysm, blocking off blood flow into the aneurysm sac.
2. Redirection of Flow: The flow diverter redirects blood flow along the normal artery, leading to a decrease in pressure inside the aneurysm. Over time, this causes thrombosis (clotting) inside the aneurysm, which results in the eventual obliteration of the aneurysm.
Step 2: Indications for Use:
1. Complex Aneurysms: Flow diverters are primarily used in the treatment of large, wide-necked, or fusiform aneurysms that are not amenable to conventional coiling or clipping.
2. Unruptured Aneurysms: They are typically used for unruptured aneurysms, especially in areas that are difficult to treat with traditional methods.
3. Recurrent Aneurysms: In cases where previous treatments (such as coiling) have failed, flow diverters can be used to treat recanalized aneurysms.
Step 3: Benefits and Limitations:
1. Benefits: Flow diverters offer a minimally invasive approach to treating difficult aneurysms, with a high rate of aneurysm obliteration. They are particularly useful for aneurysms in challenging locations, such as the internal carotid artery.
2. Limitations: The major limitation of flow diverters is the potential for complications, such as thromboembolic events, and the risk of delayed rupture. Furthermore, the procedure requires a highly skilled interventional team and may not be suitable for all patients. Quick Tip: Flow diverters are a highly effective treatment option for complex aneurysms, particularly those with wide necks, but careful patient selection and monitoring are essential.
Indications for carotid endarterectomy.
View Solution
Carotid endarterectomy (CEA) is a surgical procedure used to remove atherosclerotic plaques from the carotid arteries to prevent stroke. It is typically performed in patients with symptomatic or asymptomatic carotid stenosis to reduce the risk of stroke.
Step 1: Indications for Carotid Endarterectomy:
1. Symptomatic Carotid Stenosis: CEA is indicated for patients with symptomatic carotid stenosis (i.e., those who have had a transient ischemic attack or stroke due to the stenosis) with a greater than 50% narrowing of the carotid artery. The procedure reduces the risk of recurrent stroke in these patients.
2. Asymptomatic Carotid Stenosis: CEA may also be performed in patients with asymptomatic carotid stenosis, especially if the stenosis is greater than 70%, in order to reduce the risk of future stroke. This decision is made based on individual risk factors and the patient's overall health.
3. High-Risk Features: CEA may be considered in patients with high-risk features, such as a history of contralateral stroke or significant progression of stenosis despite medical therapy.
Step 2: Preoperative Evaluation:
1. Imaging Studies: Patients considered for CEA should undergo carotid ultrasound, CT angiography, or MR angiography to accurately assess the degree of stenosis and plaque morphology.
2. Cardiac Evaluation: A cardiac evaluation is essential to assess for any contraindications to surgery, such as uncontrolled arrhythmias or heart disease.
Step 3: Contraindications to Carotid Endarterectomy:
1. Severe Medical Comorbidities: CEA is generally not recommended for patients with severe comorbidities that would increase the risk of surgery, such as end-stage renal disease or advanced cancer.
2. Total Occlusion: Carotid endarterectomy is not effective in patients with complete occlusion of the carotid artery, as the procedure would not improve blood flow to the brain.
3. High Surgical Risk: Patients with a high risk of perioperative complications, such as those with severe pulmonary or cardiac disease, may not be suitable candidates for CEA. Quick Tip: Carotid endarterectomy is a proven procedure for preventing stroke in patients with symptomatic or severe asymptomatic carotid stenosis, but patient selection is key to ensuring optimal outcomes.
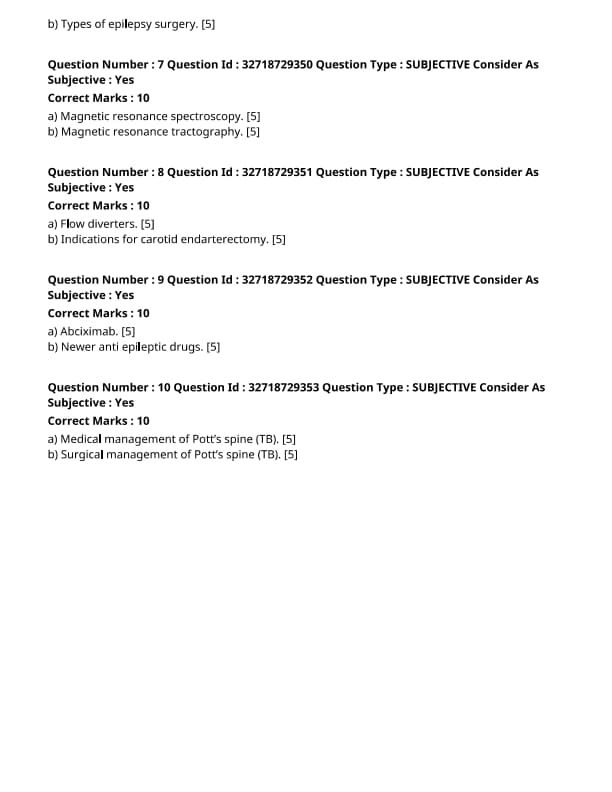
Abciximab.
View Solution
Abciximab is a monoclonal antibody that is used as an antiplatelet drug to prevent thrombosis in patients undergoing coronary angioplasty or stent placement. It is a glycoprotein IIb/IIIa inhibitor that prevents platelet aggregation.
Step 1: Mechanism of Action:
1. Inhibition of Platelet Aggregation: Abciximab binds to the glycoprotein IIb/IIIa receptor on the surface of platelets, preventing fibrinogen from binding and inhibiting platelet aggregation.
2. Prevention of Thrombosis: By blocking platelet aggregation, abciximab helps reduce the risk of thrombus formation, which can lead to complications such as myocardial infarction or stroke during percutaneous coronary interventions (PCI).
Step 2: Clinical Applications:
1. Acute Coronary Syndromes (ACS): Abciximab is commonly used in the management of ACS, including unstable angina and non-ST-segment elevation myocardial infarction (NSTEMI).
2. Percutaneous Coronary Intervention (PCI): It is used during PCI procedures to prevent thrombotic complications, particularly in patients with high-risk coronary artery disease.
Step 3: Side Effects:
1. Bleeding: The most common side effect is bleeding due to its antiplatelet activity.
2. Thrombocytopenia: Rarely, abciximab can cause thrombocytopenia, which may require discontinuation of the drug.
3. Allergic Reactions: Some patients may experience allergic reactions to the drug, including rash, fever, or more severe reactions.
Step 4: Contraindications:
1. Active Bleeding: Abciximab should not be used in patients with active bleeding or a history of bleeding disorders.
2. Severe Hypertension: It is contraindicated in patients with uncontrolled hypertension, as the risk of bleeding is increased. Quick Tip: Abciximab is an effective antiplatelet agent for reducing thrombotic complications during PCI but must be used with caution due to its bleeding risk.
Newer anti-epileptic drugs.
View Solution
Newer anti-epileptic drugs (AEDs) are used to treat epilepsy, particularly in patients who are refractory to older treatments. These drugs have been developed to provide better control of seizures with fewer side effects and drug interactions.
Step 1: Common Newer Anti-Epileptic Drugs:
1. Levetiracetam: A commonly used AED, levetiracetam works by modulating neurotransmitter release and has a broad spectrum of activity, making it effective for many types of seizures. It has fewer drug interactions compared to older AEDs.
2. Lamotrigine: Lamotrigine is used to treat both focal and generalized seizures. It works by inhibiting sodium channels, thus stabilizing neuronal membranes and preventing excessive neuronal firing.
3. Topiramate: Topiramate is effective in treating focal and generalized seizures. It has multiple mechanisms of action, including the inhibition of glutamate receptors and enhancement of GABA activity.
4. Gabapentin: Gabapentin is effective for partial seizures and is often used as an adjunctive therapy for neuropathic pain. It works by binding to calcium channels and modulating excitability.
5. Zonisamide: Zonisamide is effective for focal and generalized seizures and is thought to work by inhibiting sodium and calcium channels.
Step 2: Advantages of Newer AEDs:
1. Fewer Side Effects: Newer AEDs generally have a more favorable side-effect profile compared to older medications, such as phenytoin or carbamazepine.
2. Fewer Drug Interactions: Newer AEDs tend to have fewer interactions with other drugs, which is beneficial for patients on polypharmacy.
3. Ease of Use: Many newer AEDs come in once-daily formulations, improving patient adherence to treatment.
Step 3: Limitations:
1. Cost: Newer AEDs tend to be more expensive than older drugs, which may be a limiting factor in their use.
2. Long-Term Safety: Although these drugs have been shown to be effective in clinical trials, the long-term safety data is still evolving.
3. Side Effects: While generally better tolerated, newer AEDs can still cause side effects like dizziness, fatigue, or cognitive impairment. Quick Tip: Newer anti-epileptic drugs offer significant benefits in seizure control and patient safety but should be used judiciously, especially considering their cost and long-term safety.
Medical management of Pott’s spine (TB).
View Solution
Step 1: Understanding Pott’s Spine:
Pott’s spine refers to tuberculosis (TB) of the spine, which is a form of osteomyelitis. It typically affects the vertebral bodies and can lead to severe complications, including spinal deformities, neurological deficits, and paralysis.
Step 2: Medical Management of Pott’s Spine:
1. Anti-Tuberculosis Therapy: The cornerstone of medical management is the administration of anti-tuberculosis drugs. The standard regimen typically includes a combination of Rifampicin, Isoniazid, Pyrazinamide, and Ethambutol for at least 6-12 months. The duration may vary based on clinical response.
2. Supportive Care: Adequate bed rest is essential to prevent further spinal damage. Pain management with analgesics and anti-inflammatory medications is important.
3. Nutritional Support: Proper nutrition is necessary to support the immune system and overall recovery.
4. Monitoring for Complications: Regular follow-up is necessary to assess the effectiveness of the treatment, monitor for side effects of medications, and prevent or detect complications such as spinal deformities and neurological impairment.
5. Adjunctive Therapy: In cases with significant inflammation, corticosteroids may be used to reduce swelling and pain. Quick Tip: Anti-tuberculosis therapy is crucial in managing Pott's spine, and early intervention is key to preventing long-term complications.
Surgical management of Pott’s spine (TB).
View Solution
Step 1: Indications for Surgery in Pott’s Spine:
Surgical intervention is required in certain cases where medical management alone is insufficient or if there are complications. Indications for surgery include:
1. Neurological Deficits: If there is progressive neurological impairment due to spinal cord compression or abscess formation.
2. Spinal Deformities: Severe kyphosis or spinal instability that affects function or causes pain.
3. Failure of Medical Therapy: If there is inadequate response to anti-TB medications after an appropriate duration of therapy.
4. Abscess Drainage: In cases of paraspinal or epidural abscess formation.
Step 2: Surgical Procedures:
1. Debridement and Drainage: Surgical removal of necrotic tissue and drainage of abscesses may be necessary in cases with large paraspinal or epidural abscesses.
2. Spinal Fusion: In cases of spinal instability or severe deformities, spinal fusion may be performed to stabilize the affected vertebrae.
3. Decompression: If there is significant compression of the spinal cord, decompression surgery may be performed to relieve pressure and prevent further neurological damage.
4. Postoperative Care: After surgery, immobilization with a brace or external support is usually required to ensure proper healing and prevent further complications. Quick Tip: Surgical management is typically reserved for cases with neurological impairment or severe deformity, with a focus on relieving pressure and stabilizing the spine.




Comments