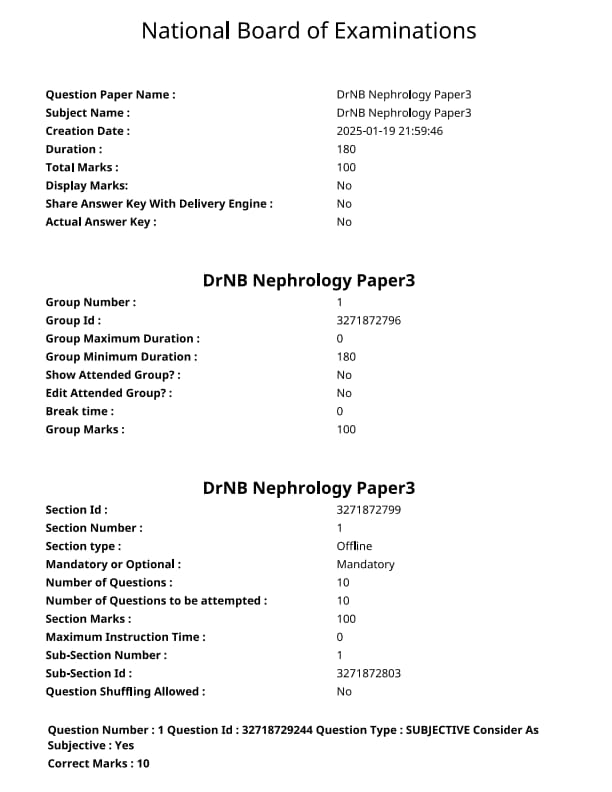
NEET SS 2024 DrNB Nephrology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Nephrology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Nephrology Paper 3 Question Paper | Check Solutions |

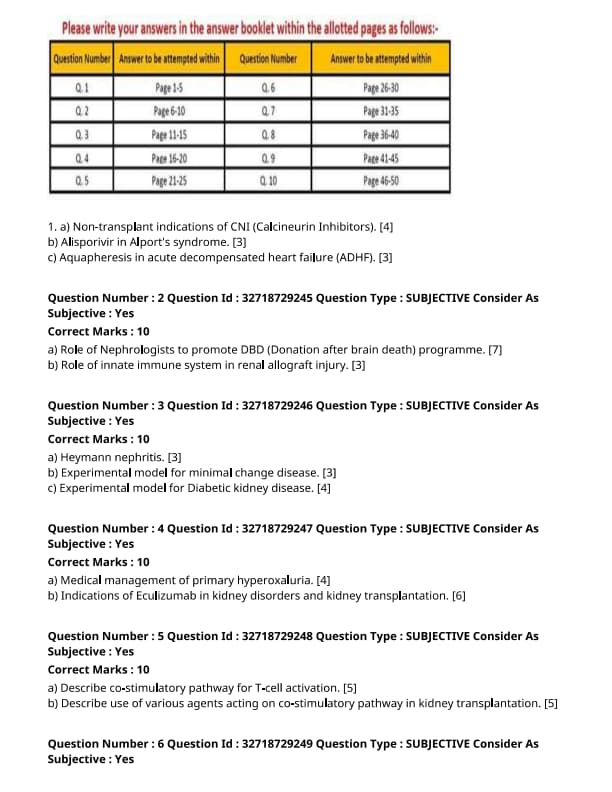
Non-transplant indications of CNI (Calcineurin Inhibitors).
View Solution
Calcineurin inhibitors (CNIs), such as tacrolimus and cyclosporine, are primarily used in organ transplantation to prevent graft rejection. However, they also have non-transplant indications due to their immunosuppressive properties.
Step 1: Non-transplant Indications:
1. Autoimmune Diseases: CNIs are used in the treatment of various autoimmune disorders, including systemic lupus erythematosus (SLE) and rheumatoid arthritis, to suppress immune system activity and reduce inflammation.
2. Nephrotic Syndrome: CNIs can be used in steroid-resistant nephrotic syndrome, especially in children, to reduce proteinuria and improve kidney function.
3. Dermatologic Conditions: Tacrolimus is commonly used in the form of topical ointments for atopic dermatitis and psoriasis to reduce inflammation and control symptoms.
Step 2: Mechanism of Action:
CNIs inhibit calcineurin, a protein phosphatase that activates T-cells by dephosphorylating nuclear factors. This suppression of T-cell activation decreases the production of cytokines, leading to reduced inflammation. Quick Tip: While effective for autoimmune diseases, CNIs should be used cautiously due to their potential nephrotoxic and neurotoxic effects.
Alisporivir in Alport's syndrome.
View Solution
Alisporivir is an antiviral drug primarily used in the treatment of hepatitis C. However, its use in Alport’s syndrome is being explored due to its potential role in treating associated renal complications.
Step 1: Mechanism of Action:
Alisporivir is a cyclosporine derivative that inhibits the hepatitis C virus (HCV) NS5A protein. It also has immunosuppressive properties, which may be beneficial in reducing glomerular damage in Alport’s syndrome.
Step 2: Role in Alport’s Syndrome:
1. Renal Protection: Alisporivir may reduce proteinuria and protect against further kidney damage by modulating immune responses in the kidneys.
2. Clinical Trials: Early clinical studies suggest that alisporivir may help improve renal outcomes in patients with Alport’s syndrome, especially in those with significant proteinuria.
Step 3: Challenges and Future Directions:
1. Safety and Efficacy: More research is needed to assess the long-term safety and effectiveness of alisporivir in Alport’s syndrome, as well as its impact on renal function and progression to end-stage renal disease. Quick Tip: Alisporivir is an emerging therapy for Alport’s syndrome, but its use is still under investigation and should be considered with caution.
Aquapheresis in acute decompensated heart failure (ADHF).
View Solution
Aquapheresis, also known as ultrafiltration, is a process used to remove excess fluid from the body in patients with acute decompensated heart failure (ADHF).
Step 1: Mechanism of Action:
Aquapheresis works by using a machine to filter excess fluid from the blood, which is then removed via a catheter. This procedure helps alleviate symptoms of fluid overload, such as pulmonary edema, in patients with heart failure.
Step 2: Indications for Aquapheresis:
1. Fluid Overload in ADHF: It is primarily used in patients with severe ADHF who are not responding adequately to diuretics.
2. Diuretic Resistance: In patients with diuretic resistance, aquapheresis can be a useful alternative to help remove excess fluid.
Step 3: Benefits and Risks:
1. Benefits: Aquapheresis can improve hemodynamics, reduce symptoms of congestion, and improve exercise capacity.
2. Risks: Potential risks include hypotension, electrolyte imbalances, and vascular complications due to the catheter. Quick Tip: Aquapheresis is an effective option for managing fluid overload in ADHF, particularly when diuretics fail, but it requires careful monitoring of the patient.
Role of Nephrologists to promote DBD (Donation after brain death) programme.
View Solution
Nephrologists play a crucial role in promoting the DBD (Donation after Brain Death) program, which is essential for organ donation and transplantation, particularly in cases of kidney transplantation. Their involvement helps ensure that organ donation is ethically managed, efficiently organized, and done with optimal patient outcomes.
Step 1: Identifying Potential Donors:
1. Screening Brain Dead Patients: Nephrologists can help identify brain-dead patients who are potential organ donors. This includes assessing kidney function and other organ viability.
2. Early Intervention: Prompt recognition of brain death and early consultation with organ procurement organizations (OPOs) are crucial in maintaining organ function until transplantation.
Step 2: Educating and Raising Awareness:
1. Awareness Campaigns: Nephrologists can advocate for organ donation by educating the public, patients, and families about the benefits of DBD.
2. Patient and Family Support: Providing counseling to families of potential organ donors about brain death and the donation process, ensuring that their wishes are respected.
Step 3: Ensuring Optimal Organ Function:
1. Managing Organ Preservation: Nephrologists are responsible for the management of kidney function in brain-dead patients, including maintaining proper hydration, electrolytes, and renal perfusion.
2. Preventing Organ Dysfunction: Proactively managing blood pressure, infection, and other factors that may compromise organ viability prior to procurement.
Step 4: Collaboration and Coordination:
1. Collaboration with Transplant Teams: Nephrologists play an essential role in collaborating with transplant surgeons and organ procurement teams to ensure smooth organ retrieval and transplantation processes.
2. Post-transplant Care: Nephrologists may also be involved in the care of kidney transplant recipients, ensuring the transplanted kidney functions properly. Quick Tip: Nephrologists are key to promoting the DBD program, not only in identifying potential donors but also in optimizing organ function and educating patients and families.
Role of innate immune system in renal allograft injury.
View Solution
The innate immune system plays a significant role in renal allograft injury, particularly in the early stages following kidney transplantation. It can contribute to both the immediate and delayed rejection of the transplanted kidney and influence graft survival.
Step 1: Mechanisms of Injury:
1. Activation of Innate Immunity: Upon kidney transplantation, the recipient's immune system detects the graft as foreign, triggering an innate immune response. This involves the activation of pattern recognition receptors (PRRs) like toll-like receptors (TLRs) on immune cells.
2. Inflammatory Response: Activation of the innate immune system leads to the release of pro-inflammatory cytokines, which recruit neutrophils and macrophages to the graft site, causing inflammation and injury to renal tissue.
Step 2: Early Post-Transplant Inflammation:
1. Ischemia-Reperfusion Injury (IRI): During transplantation, periods of ischemia followed by reperfusion can exacerbate innate immune activation, leading to further renal injury.
2. DAMPs and PAMPs: Damage-associated molecular patterns (DAMPs) from the graft and pathogen-associated molecular patterns (PAMPs) from infection can activate innate immune receptors, contributing to graft damage.
Step 3: Role of Innate Immune Cells:
1. Macrophages: Macrophages are central to the innate immune response and can either exacerbate injury by promoting inflammation or resolve it through anti-inflammatory cytokines. Their polarization into M1 or M2 macrophages can determine the extent of graft damage.
2. Neutrophils: Neutrophils contribute to early renal injury, particularly in the setting of IRI, by releasing enzymes and reactive oxygen species that damage kidney cells.
Step 4: Strategies to Modulate the Innate Immune Response:
1. Immunosuppressive Therapy: While primarily aimed at adaptive immune responses, immunosuppressive drugs can also influence innate immunity by modulating inflammation.
2. Targeting Inflammatory Pathways: Targeting specific innate immune pathways, such as TLRs or cytokines like IL-1, may offer new strategies for reducing allograft injury and improving graft survival. Quick Tip: The innate immune system plays a crucial role in renal allograft injury, and understanding its mechanisms offers potential for improving post-transplant outcomes.
Heymann nephritis.
View Solution
Heymann nephritis is an experimental autoimmune model of nephritis that mimics human membranous nephropathy. It is induced by immunization with a protein found in the glomerular basement membrane, leading to the formation of immune complexes that deposit in the glomeruli.
Step 1: Pathogenesis of Heymann Nephritis:
1. Immunization: The model is induced in animals, typically rats, by injecting them with a renal antigen (megalin) extracted from the proximal tubular cells of the kidneys. The immune response to this antigen leads to the formation of antibodies.
2. Immune Complex Deposition: The antibodies formed against the antigen bind to the glomerular basement membrane, forming immune complexes. These complexes deposit along the glomerular capillaries, triggering an inflammatory response.
3. Inflammation and Proteinuria: The immune complexes activate complement and attract inflammatory cells, leading to glomerular injury, which results in proteinuria and nephrotic syndrome in the animal model.
Step 2: Clinical Relevance:
1. Human Relevance: Heymann nephritis serves as a model for human membranous nephropathy, a condition characterized by thickening of the glomerular basement membrane and the presence of immune complexes.
2. Use in Research: The model helps to study the pathogenesis of glomerular diseases and test potential therapeutic interventions for treating nephrotic syndrome and autoimmune renal diseases. Quick Tip: Heymann nephritis is a valuable experimental model for studying autoimmune kidney diseases like membranous nephropathy.
Experimental model for minimal change disease.
View Solution
Minimal change disease (MCD) is a common cause of nephrotic syndrome, especially in children. While the exact cause of MCD is unknown, an experimental model of the disease is used to understand its pathogenesis and develop therapeutic strategies.
Step 1: Experimental Model for Minimal Change Disease:
1. Induction of MCD in Animals: The most widely used animal model for minimal change disease is the administration of nephrotoxic agents, such as puromycin aminonucleoside (PAN), to rats or mice.
2. Pathogenesis: PAN induces foot process effacement in podocytes, which is the hallmark of MCD in humans. The mechanism is thought to involve damage to the glomerular filtration barrier, leading to protein leakage into the urine.
3. Proteinuria: Animals injected with PAN develop massive proteinuria, similar to human MCD. The model is used to investigate the role of podocytes in maintaining the filtration barrier and the involvement of immune mechanisms in disease progression.
Step 2: Research Applications:
1. Drug Testing: The PAN-induced MCD model is valuable for testing potential treatments for nephrotic syndrome, including corticosteroids and immunosuppressive agents.
2. Mechanistic Studies: Researchers use this model to explore the role of cytokines, podocyte signaling pathways, and immune system involvement in the development of MCD. Quick Tip: The PAN-induced model is a widely used experimental system to study the pathophysiology and treatment of minimal change disease.
Experimental model for Diabetic Kidney Disease.
View Solution
Diabetic kidney disease (DKD) is a common complication of diabetes and is a leading cause of end-stage renal disease. The development of experimental models of DKD allows researchers to study its pathophysiology and test therapeutic interventions.
Step 1: Experimental Models of Diabetic Kidney Disease:
1. Streptozotocin (STZ)-Induced Diabetes: The most widely used animal model for DKD is the induction of diabetes using streptozotocin (STZ), a toxin that selectively destroys pancreatic beta cells, leading to hyperglycemia and insulin deficiency.
2. Pathophysiology: STZ-induced diabetic animals develop several features of DKD, including glomerular hypertrophy, increased albuminuria, and changes in the glomerular basement membrane. These changes mimic the pathophysiological alterations seen in humans with diabetic nephropathy.
3. Genetic Models: Genetically modified animals, such as the db/db mouse (obesity and type 2 diabetes model), are also used to study DKD. These animals develop insulin resistance and kidney damage similar to human diabetic nephropathy.
Step 2: Research Applications:
1. Pathway Studies: These models are used to study the molecular mechanisms underlying diabetic kidney disease, including the role of advanced glycation end-products (AGEs), inflammation, and fibrosis.
2. Drug Development: Animal models of DKD are essential for evaluating new drugs aimed at slowing the progression of diabetic nephropathy, such as angiotensin receptor blockers (ARBs), SGLT2 inhibitors, and other renoprotective agents. Quick Tip: STZ-induced and genetic models of diabetes are crucial for studying diabetic kidney disease and testing potential therapeutic interventions.
Medical management of primary hyperoxaluria.
View Solution
Primary hyperoxaluria is a rare genetic disorder characterized by excessive oxalate production, leading to kidney stones, nephrocalcinosis, and progressive renal failure. The medical management of primary hyperoxaluria focuses on reducing oxalate production and promoting its excretion.
Step 1: General Principles:
1. Adequate Hydration: Ensuring sufficient fluid intake is essential to prevent the formation of oxalate crystals and kidney stones. Increased urinary volume dilutes the oxalate concentration and reduces the risk of stone formation.
2. Dietary Modifications: Restricting dietary oxalate and increasing calcium intake may help to reduce oxalate absorption in the gastrointestinal tract.
3. Use of Pyridoxine: Pyridoxine (vitamin B6) is used in some forms of primary hyperoxaluria, particularly type 1, where it helps to reduce oxalate production by increasing the activity of the enzyme alanine-glyoxylate aminotransferase (AGT).
Step 2: Pharmacological Treatment:
1. Thiazide Diuretics: Thiazide diuretics can reduce urinary calcium excretion and prevent calcium oxalate stone formation by reducing the amount of free calcium in the urine.
2. Potassium Citrate: Potassium citrate is used to increase urinary citrate levels, which inhibits stone formation and helps to bind excess calcium in the urine, preventing crystallization of calcium oxalate.
3. Oxalate-Binding Agents: Agents such as calcium carbonate or magnesium may be used to bind dietary oxalate in the intestines and reduce its absorption.
Step 3: Renal Replacement Therapy:
1. Dialysis: In cases of progressive kidney failure, dialysis may be required to manage the accumulation of toxins, including oxalate.
2. Kidney Transplantation: In severe cases, where kidney function deteriorates significantly, a kidney transplant may be necessary. However, the transplanted kidney may also be at risk of oxalate deposition.
Step 4: Liver Transplantation:
In cases of severe hyperoxaluria, liver transplantation may be considered. Since the liver is responsible for the production of oxalate, a liver transplant can provide a definitive treatment by correcting the underlying metabolic defect. Quick Tip: Early diagnosis and aggressive management of primary hyperoxaluria are key to preventing irreversible kidney damage and improving patient outcomes.
Indications of Eculizumab in kidney disorders and kidney transplantation.
View Solution
Eculizumab is a monoclonal antibody that inhibits complement protein C5, thereby preventing the activation of the complement system. It is used to treat several kidney disorders and to improve outcomes in kidney transplantation by modulating the immune response.
Step 1: Kidney Disorders Treated with Eculizumab:
1. Atypical Hemolytic Uremic Syndrome (aHUS): Eculizumab is used in the treatment of aHUS, a rare but life-threatening disorder characterized by the formation of small blood clots in the kidneys, leading to renal injury and failure. By inhibiting complement activation, eculizumab prevents further kidney damage.
2. Paroxysmal Nocturnal Hemoglobinuria (PNH): Eculizumab is used to treat PNH, a condition in which red blood cells are destroyed by the complement system, leading to hemolysis and kidney damage. Eculizumab reduces hemolysis and improves kidney function.
Step 2: Role of Eculizumab in Kidney Transplantation:
1. Prevention of Acute Rejection: Eculizumab has been studied in the context of kidney transplantation to prevent acute rejection, particularly in patients who have developed antibody-mediated rejection (AMR). By inhibiting complement activation, it can help reduce tissue injury and improve graft survival.
2. Prevention of Antibody-Mediated Rejection (AMR): In patients who have pre-formed antibodies against the donor organ, eculizumab can reduce complement-mediated injury and improve graft function, especially in sensitized patients or those with high-risk HLA mismatches.
Step 3: Side Effects and Limitations:
1. Infections: One of the most significant risks of eculizumab therapy is the increased risk of infections, particularly meningococcal infections. Vaccination against Neisseria meningitidis is recommended before starting treatment.
2. Cost: Eculizumab is a costly medication, and its use may be limited by healthcare resources and insurance coverage.
Step 4: Long-Term Use:
Eculizumab is generally used for long-term management of conditions like aHUS and PNH, but its use in kidney transplantation is typically short-term, focused on preventing rejection in the early postoperative period. Quick Tip: Eculizumab is a powerful complement inhibitor with important therapeutic applications in kidney disorders and transplantation, but it requires careful monitoring due to the risk of infections.
Describe co-stimulatory pathway for T-cell activation.
View Solution
Step 1: Overview of T-Cell Activation:
T-cell activation is a critical process in immune responses. The activation requires two signals: the primary signal is provided by the T-cell receptor (TCR) interacting with the peptide-MHC complex on antigen-presenting cells (APCs), and the secondary signal is provided by co-stimulatory molecules. Without the co-stimulatory signal, T-cell activation is incomplete, and the T-cell may undergo anergy or apoptosis.
Step 2: Co-Stimulatory Pathway for T-Cell Activation:
The key co-stimulatory pathways include:
1. CD28 and B7 Interaction: The interaction between CD28 (on T-cells) and B7 molecules (on APCs) is the primary co-stimulatory signal. This binding results in the full activation of T-cells and promotes cytokine production.
2. ICOS and ICOS-L Interaction: Inducible T-cell co-stimulator (ICOS) on activated T-cells interacts with ICOS ligand (ICOS-L) on APCs. This pathway plays a critical role in the differentiation of T-helper cells and the maintenance of immune responses.
3. CD40 and CD40L Interaction: The interaction between CD40 (on APCs) and CD40 ligand (CD40L) (on T-cells) is important in the activation of APCs and in promoting the T-helper cell response.
4. CD137 (4-1BB) and CD137L Interaction: CD137 (a member of the TNF receptor family) interacts with CD137L on APCs, enhancing T-cell proliferation and cytokine production.
Step 3: Regulatory Co-Stimulatory Pathways:
In addition to positive co-stimulatory signals, there are negative co-stimulatory pathways that regulate T-cell responses:
1. CTLA-4 and B7 Interaction: CTLA-4 (Cytotoxic T-Lymphocyte Antigen-4) competes with CD28 for binding to B7, delivering an inhibitory signal that limits T-cell activation.
2. PD-1 and PD-L1/PD-L2 Interaction: The interaction of PD-1 (Programmed Cell Death Protein 1) with its ligands (PD-L1/PD-L2) on APCs and tumor cells leads to T-cell exhaustion, a mechanism to prevent autoimmunity. Quick Tip: Co-stimulatory signals are essential for T-cell activation, and disruptions in these pathways can lead to immune dysfunction, including autoimmunity or immunodeficiency.
Describe use of various agents acting on co-stimulatory pathway in kidney transplantation.
View Solution
Step 1: Co-Stimulatory Pathways in Kidney Transplantation:
In kidney transplantation, co-stimulatory pathways play a crucial role in the immune response to the transplanted organ. T-cell activation, which leads to allograft rejection, is dependent on co-stimulatory signals between T-cells and APCs. Modulating these pathways can help prevent rejection and promote graft tolerance.
Step 2: Agents Acting on Co-Stimulatory Pathways in Kidney Transplantation:
1. CTLA-4 Ig (Abatacept): Abatacept is a fusion protein that blocks the interaction between CD28 and B7, preventing the co-stimulatory signal necessary for T-cell activation. It is used in kidney transplantation to prevent acute rejection.
2. Belatacept: Similar to abatacept, belatacept is a modified version of CTLA-4 Ig that has been shown to reduce the incidence of acute rejection and improve long-term graft survival in kidney transplant recipients.
3. Anti-PD-1/PD-L1 Therapy: Agents targeting the PD-1/PD-L1 pathway, like nivolumab and pembrolizumab, are being explored to enhance graft tolerance and reduce rejection by inhibiting the T-cell exhaustion pathway.
4. Anti-CD40 and Anti-CD40L Therapy: Blocking the CD40-CD40L interaction between T-cells and APCs can prevent allograft rejection and improve long-term graft survival. Agents like anti-CD40 monoclonal antibodies are under investigation in clinical trials.
5. Toll-Like Receptor (TLR) Inhibitors: TLRs are involved in the activation of APCs and the initiation of immune responses. Inhibitors of TLRs may help reduce graft rejection by modulating the immune response.
Step 3: Potential Side Effects and Challenges:
1. Infection Risk: Modulation of co-stimulatory pathways can increase the risk of infections due to immunosuppression.
2. Tumorigenesis: Long-term inhibition of co-stimulatory signals may increase the risk of malignancies due to impaired immune surveillance.
3. Dosing and Safety: Proper dosing and monitoring are essential to balance graft protection with the risk of excessive immune suppression. Quick Tip: Agents targeting co-stimulatory pathways offer promise in preventing kidney transplant rejection, but the balance between preventing rejection and maintaining immune function is critical.
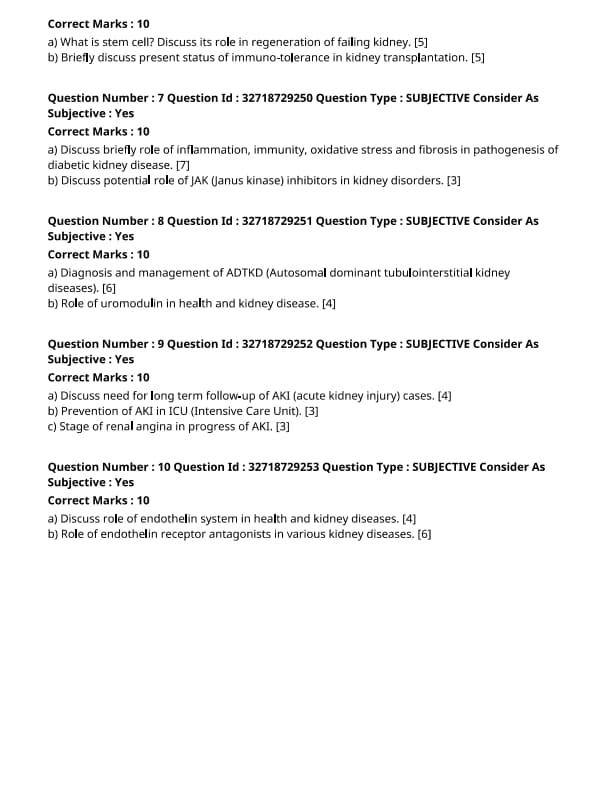
What is stem cell? Discuss its role in regeneration of failing kidney.
View Solution
Stem cells are undifferentiated cells that have the potential to develop into various specialized cell types in the body. They are capable of self-renewal and can divide to produce both identical stem cells and differentiated cells. Stem cells can be classified into two main types: embryonic stem cells (ESCs) and adult stem cells (somatic stem cells).
Step 1: Types of Stem Cells:
1. Embryonic Stem Cells (ESCs): Pluripotent cells derived from early-stage embryos, capable of differentiating into all cell types.
2. Adult Stem Cells: Multipotent cells found in specific tissues (e.g., bone marrow, skin, kidneys) that can differentiate into a limited range of cell types related to their tissue of origin.
Step 2: Stem Cells in Kidney Regeneration:
1. Stem Cells for Repairing Kidney Tissue: Stem cells, especially those from the bone marrow or induced pluripotent stem cells (iPSCs), have been explored for their potential to regenerate damaged kidney tissue in chronic kidney disease (CKD).
2. Kidney Progenitor Cells: Recent studies suggest that kidney progenitor cells can differentiate into nephron cells (e.g., podocytes, tubular cells) and contribute to tissue repair in response to injury or degeneration.
3. Potential for Kidney Disease Treatment: Stem cell therapy may provide a promising approach to treat kidney failure by stimulating tissue repair, improving kidney function, and potentially reducing the need for dialysis or transplants.
Step 3: Challenges and Considerations:
1. Ethical Concerns: The use of ESCs raises ethical concerns due to the need for embryos, while adult stem cells face fewer ethical issues.
2. Immune Rejection: Stem cells from foreign sources may be subject to immune rejection unless carefully matched or modified.
3. Clinical Translation: More research and clinical trials are needed to assess the long-term effectiveness and safety of stem cell therapies in kidney regeneration. Quick Tip: Stem cell therapy holds great promise for regenerating damaged kidney tissue, but significant challenges remain in terms of safety, efficacy, and ethical considerations.
Briefly discuss present status of immuno-tolerance in kidney transplantation.
View Solution
Immuno-tolerance in kidney transplantation refers to the ability of the recipient’s immune system to accept the transplanted kidney without rejecting it, even in the absence of immunosuppressive drugs.
Step 1: Mechanism of Immuno-tolerance:
1. Induction of Tolerance: Immuno-tolerance can be induced through various strategies, such as the use of tolerogenic dendritic cells or regulatory T cells that suppress immune responses against the graft.
2. Chimerism: In some cases, donor-specific chimerism (presence of donor-derived immune cells) has been shown to promote tolerance of the transplanted organ.
Step 2: Current Approaches to Achieve Immuno-tolerance:
1. Targeted Immunosuppressive Therapy: Strategies involving specific immunosuppressive drugs (e.g., rapamycin, calcineurin inhibitors) aim to suppress the immune response while promoting tolerance.
2. Regulatory T Cell Expansion: Expanding and infusing regulatory T cells into transplant recipients can help induce long-term tolerance and reduce reliance on conventional immunosuppressive drugs.
3. Mixed Chimerism: Some studies are exploring the use of mixed chimerism to promote immune tolerance, where the recipient's immune system is re-educated to accept the transplanted kidney as its own.
Step 3: Challenges and Future Directions:
1. Risk of Infection and Cancer: Long-term immuno-tolerance may expose the recipient to increased risks of infection and malignancy due to the suppressed immune response.
2. Durability of Tolerance: Maintaining stable tolerance over time remains a challenge, and further research is needed to ensure the long-term success of immuno-tolerance strategies.
3. Personalized Approaches: Future therapies may involve personalized medicine, tailoring immuno-tolerance induction strategies based on genetic and immunological factors specific to each transplant recipient. Quick Tip: Immuno-tolerance offers a promising future for kidney transplantation, reducing the need for lifelong immunosuppressive drugs and improving long-term outcomes.
Discuss briefly the role of inflammation, immunity, oxidative stress, and fibrosis in the pathogenesis of diabetic kidney disease.
View Solution
Diabetic kidney disease (DKD) is a major complication of diabetes and contributes significantly to the burden of chronic kidney disease. Several pathological mechanisms, including inflammation, immune responses, oxidative stress, and fibrosis, play a key role in the development and progression of DKD.
Step 1: Inflammation and Immunity:
1. Inflammatory Pathways: In DKD, hyperglycemia leads to the activation of inflammatory pathways, including the production of pro-inflammatory cytokines (such as TNF-alpha and IL-6) and chemokines, which recruit immune cells to the kidneys.
2. Immune Cells: Activated macrophages, T-cells, and dendritic cells contribute to glomerular and tubular damage by releasing inflammatory mediators. This inflammation exacerbates endothelial dysfunction, leading to glomerulosclerosis and tubulointerstitial fibrosis.
Step 2: Oxidative Stress:
1. Increased ROS Production: Chronic hyperglycemia in diabetes leads to increased production of reactive oxygen species (ROS) in renal cells, particularly through the activation of the NADPH oxidase pathway.
2. Renal Cell Injury: ROS cause damage to renal cells, including podocytes, endothelial cells, and mesangial cells, by inducing DNA damage, lipid peroxidation, and protein modification. This further promotes inflammation and fibrosis.
Step 3: Fibrosis:
1. Extracellular Matrix (ECM) Accumulation: In response to chronic injury, there is excessive deposition of extracellular matrix components (such as collagen) in the kidneys.
2. Activation of Fibrotic Pathways: Transforming growth factor-beta (TGF-beta) is a key mediator in fibrosis, promoting the differentiation of fibroblasts into myofibroblasts, which secrete collagen and contribute to renal scarring.
3. Progression to End-Stage Renal Disease (ESRD): The accumulation of fibrotic tissue leads to glomerulosclerosis, tubular atrophy, and ultimately kidney failure in patients with DKD.
Step 4: Role of Metabolic and Hemodynamic Factors:
1. Hyperglycemia and Hypertension: Both factors are key contributors to the pathogenesis of DKD, driving the inflammatory and fibrotic processes.
2. Renal Hyperfiltration: Early in the disease, the kidneys undergo hyperfiltration, which contributes to glomerular hypertension and increases the risk of glomerulosclerosis. Quick Tip: In diabetic kidney disease, targeting inflammation, oxidative stress, and fibrosis may help in halting the progression of the disease and improving kidney function.
Discuss the potential role of JAK (Janus kinase) inhibitors in kidney disorders.
View Solution
Janus kinases (JAKs) are a family of intracellular enzymes involved in the signaling of several cytokines and growth factors. JAK inhibitors have shown promise in modulating immune responses and inflammatory pathways, making them a potential therapeutic option in various kidney disorders.
Step 1: JAK-STAT Pathway in Kidney Disorders:
1. Cytokine Signaling: The JAK-STAT pathway is activated by a variety of cytokines, such as interferons, interleukins, and growth factors, that are implicated in the pathogenesis of kidney diseases.
2. Inflammation and Fibrosis: Inflammatory cytokines like TNF-alpha and IL-6 activate the JAK-STAT pathway, leading to the activation of immune cells and fibroblasts, which contribute to renal inflammation and fibrosis.
Step 2: Potential Role in Autoimmune Kidney Diseases:
1. Lupus Nephritis: JAK inhibitors may help in treating autoimmune kidney diseases like lupus nephritis by blocking the inflammatory signaling pathways that drive renal damage.
2. IgA Nephropathy: Recent studies suggest that JAK inhibitors may reduce the activation of the immune system and decrease proteinuria in patients with IgA nephropathy, an inflammatory kidney disease.
Step 3: Role in Diabetic Kidney Disease (DKD):
1. Inhibition of Inflammatory Pathways: JAK inhibitors may reduce the inflammatory response and fibrosis in diabetic kidney disease by inhibiting the JAK-STAT pathway, thus protecting against glomerulosclerosis and tubulointerstitial fibrosis.
2. Modulation of Renal Function: Early-stage clinical trials are exploring the effect of JAK inhibitors in preventing the progression of DKD and reducing proteinuria, a key marker of kidney damage.
Step 4: Potential Benefits and Challenges:
1. Benefits: JAK inhibitors may offer a novel approach to managing kidney disorders associated with inflammation and fibrosis, potentially improving long-term kidney outcomes.
2. Challenges: The long-term safety and efficacy of JAK inhibitors in kidney diseases are still being studied. Potential concerns include the risk of infections, malignancy, and the impact on other organ systems. Quick Tip: JAK inhibitors offer potential therapeutic benefits in treating kidney disorders by modulating inflammation and fibrosis, but further studies are needed to assess their safety and long-term efficacy.
Diagnosis and management of ADTKD (Autosomal dominant tubulointerstitial kidney diseases).
View Solution
Autosomal dominant tubulointerstitial kidney disease (ADTKD) is a group of hereditary kidney disorders characterized by progressive renal impairment due to tubulointerstitial fibrosis. ADTKD is caused by mutations in genes encoding proteins that affect renal tubular function, leading to interstitial fibrosis.
Step 1: Diagnosis of ADTKD:
1. Clinical Presentation: The symptoms of ADTKD often appear in adulthood, typically in the 3rd to 5th decade of life, with progressive kidney dysfunction, proteinuria, and hypertension. Family history plays a critical role in the diagnosis.
2. Genetic Testing: Molecular genetic testing is crucial for the diagnosis. The most common genetic mutations are found in the UMOD gene (causing uromodulin-associated kidney disease) and other genes such as MUC1 and HNF1B.
3. Histopathological Findings: On biopsy, the hallmark findings are interstitial fibrosis, tubular atrophy, and a relative lack of glomerular involvement. This helps differentiate ADTKD from other forms of kidney disease.
4. Imaging: Ultrasound or CT imaging of the kidneys may show small, shrunken kidneys, which are characteristic of chronic kidney disease in ADTKD.
Step 2: Management of ADTKD:
1. Blood Pressure Control: Strict control of blood pressure is essential to slow the progression of kidney damage. Angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs) are commonly used.
2. Management of Proteinuria: In addition to ACE inhibitors or ARBs, other measures to control proteinuria, such as sodium restriction, may be beneficial.
3. Renal Replacement Therapy: In cases where kidney function deteriorates to end-stage renal disease, renal replacement therapy such as dialysis or kidney transplantation may be required.
4. Genetic Counseling: Genetic counseling is recommended for affected families to discuss the inheritance pattern, risk of transmission, and options for prenatal diagnosis. Quick Tip: Early diagnosis and management of ADTKD can help slow the progression of kidney disease and improve quality of life.
Role of uromodulin in health and kidney disease.
View Solution
Uromodulin, also known as Tamm-Horsfall protein, is the most abundant protein in normal urine. It plays an important role in maintaining kidney function and protecting against urinary tract infections and kidney stones.
Step 1: Uromodulin in Health:
1. Urinary Protection: Uromodulin forms a protective layer in the urinary tract, preventing bacterial adhesion to the urothelium and reducing the risk of urinary tract infections.
2. Regulation of Sodium Balance: Uromodulin is involved in regulating sodium balance in the kidneys. It is secreted by the thick ascending limb of the loop of Henle and plays a role in maintaining electrolyte homeostasis.
3. Anti-inflammatory Effects: Uromodulin has anti-inflammatory properties that help protect the kidneys from injury caused by oxidative stress and inflammatory processes.
Step 2: Uromodulin in Kidney Disease:
1. Uromodulin-Associated Kidney Disease: Mutations in the UMOD gene, which encodes uromodulin, lead to autosomal dominant tubulointerstitial kidney disease (ADTKD), causing progressive kidney dysfunction due to tubulointerstitial fibrosis.
2. Kidney Stones: Uromodulin helps prevent the formation of kidney stones by inhibiting crystal aggregation. Defects in uromodulin production or function may predispose individuals to kidney stones.
3. Role in Chronic Kidney Disease (CKD): In CKD, uromodulin levels are often decreased, and its protective roles in the kidneys are compromised. Monitoring uromodulin levels may provide insights into kidney injury and disease progression.
Step 3: Potential Therapeutic Applications:
1. Gene Therapy: Genetic modification or gene therapy aimed at increasing uromodulin production may hold promise for treating diseases like ADTKD and preventing kidney damage.
2. Uromodulin-based Therapies: Research into uromodulin-based therapies is ongoing, with the goal of enhancing its protective effects in the kidneys, particularly in the context of CKD and kidney transplantation. Quick Tip: Uromodulin plays a crucial protective role in kidney function, and understanding its mechanisms could lead to new therapeutic strategies for kidney diseases.
Discuss the need for long-term follow-up of AKI (acute kidney injury) cases.
View Solution
Acute kidney injury (AKI) is a serious condition that requires immediate attention to prevent long-term kidney damage. Long-term follow-up of AKI cases is crucial to monitor renal recovery, prevent progression to chronic kidney disease (CKD), and improve overall patient outcomes.
Step 1: Risk of Progression to Chronic Kidney Disease:
1. AKI and CKD: Patients who recover from AKI are at increased risk of developing CKD, especially if the AKI episode was severe or prolonged. Regular follow-up allows early detection of any decline in kidney function.
2. Early Intervention: Early intervention can help slow or prevent the progression from AKI to CKD by optimizing blood pressure, glucose control, and kidney-friendly medications.
Step 2: Monitoring Kidney Function:
1. Serum Creatinine and eGFR: Routine monitoring of serum creatinine and estimated glomerular filtration rate (eGFR) is necessary to detect any long-term changes in kidney function.
2. Urine Protein and Albumin: Monitoring proteinuria or albuminuria can help detect kidney damage, as these are early markers of kidney injury.
Step 3: Preventing Recurrence:
1. Managing Risk Factors: Follow-up care should include managing risk factors such as hypertension, diabetes, and hyperlipidemia to reduce the risk of recurrent AKI episodes.
2. Medications and Diet: Adjusting medications, such as avoiding nephrotoxic drugs, and following a kidney-friendly diet can also help protect kidney function in the long term.
Step 4: Cardiovascular Risk Monitoring:
1. Cardiovascular Health: Patients with a history of AKI are at increased risk of cardiovascular diseases, so regular cardiovascular screening (e.g., blood pressure monitoring, lipid levels) is essential. Quick Tip: Regular follow-up of AKI patients is essential to detect early signs of CKD, prevent further kidney injury, and optimize long-term outcomes through early intervention and lifestyle changes.
Prevention of AKI in ICU (Intensive Care Unit).
View Solution
Prevention of AKI in the ICU is critical due to the high-risk nature of patients in this setting. AKI can result from various factors, including ischemia, nephrotoxins, and sepsis. Strategies to prevent AKI in the ICU focus on maintaining optimal perfusion, avoiding nephrotoxic agents, and managing underlying conditions.
Step 1: Hemodynamic Management:
1. Maintaining Adequate Blood Pressure: Ensuring sufficient renal perfusion pressure by maintaining mean arterial pressure (MAP) above 65 mmHg is essential for preventing ischemic injury.
2. Fluid Management: Proper fluid resuscitation, including the use of isotonic crystalloids, helps maintain circulatory volume and prevent prerenal causes of AKI.
Step 2: Avoiding Nephrotoxic Drugs:
1. Review Medications: Avoid the use of nephrotoxic drugs like nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics (e.g., aminoglycosides), and contrast agents, unless absolutely necessary.
2. Dose Adjustments: For necessary nephrotoxic drugs, adjust doses based on renal function to minimize the risk of damage.
Step 3: Preventing Sepsis:
1. Early Detection and Treatment: Timely identification and aggressive management of infections are crucial in preventing septic AKI, which is a common cause of AKI in the ICU.
2. Source Control: Control of infection sources, such as catheter-associated infections or abscesses, is essential to reduce the risk of sepsis-induced AKI.
Step 4: Optimizing Renal Perfusion:
1. Use of Vasopressors: In patients with hypotension or shock, vasopressors such as norepinephrine may be required to maintain blood pressure and renal perfusion.
2. Continuous Monitoring: Continuous monitoring of renal function, including urine output, serum creatinine, and urine biomarkers, allows for early detection of renal dysfunction. Quick Tip: Preventing AKI in the ICU involves careful fluid management, avoiding nephrotoxic agents, early infection control, and monitoring renal function to detect early signs of kidney injury.
Stage of renal angina in the progress of AKI.
View Solution
Renal angina is a term used to describe the early warning signs of acute kidney injury (AKI), similar to how chest pain signals myocardial ischemia. It is a clinical syndrome characterized by a combination of risk factors, symptoms, and biomarkers that indicate an increased likelihood of AKI progression.
Step 1: Staging of Renal Angina:
1. Risk Factors: Stage 1 involves patients with known risk factors for AKI, such as dehydration, use of nephrotoxic drugs, or underlying chronic kidney disease. These patients may present with mild symptoms like slight increases in serum creatinine or reduced urine output.
2. Early Detection: Stage 2 involves more pronounced symptoms and may include increased serum creatinine, reduced urine output, or the presence of early biomarkers of kidney injury (e.g., NGAL, KIM-1). Monitoring is critical to prevent progression to full-blown AKI.
3. Progression to AKI: Stage 3 involves patients with established AKI, marked by a significant rise in creatinine or a notable drop in urine output, and may require dialysis.
Step 2: Management of Renal Angina:
1. Aggressive Monitoring: Close monitoring of kidney function and early intervention to optimize perfusion and avoid nephrotoxic insults can help prevent progression from renal angina to full AKI.
2. Preventive Measures: Management includes ensuring optimal hydration, adjusting medications, and avoiding further kidney insults (e.g., nephrotoxic drugs, infection). Quick Tip: Renal angina is a clinical syndrome indicating early kidney injury, and its early recognition and management can help prevent the progression to more severe AKI.
Discuss role of endothelin system in health and kidney diseases.
View Solution
Step 1: Understanding the Endothelin System:
The endothelin (ET) system plays a critical role in regulating vascular tone, fluid balance, and tissue homeostasis. Endothelins are peptides primarily produced by endothelial cells, with the most important being endothelin-1 (ET-1). The endothelin system has two primary receptors:
1. ET-A Receptor: Predominantly involved in vasoconstriction and promoting cell proliferation.
2. ET-B Receptor: Involved in both vasodilation and vasoconstriction, depending on the tissue.
Step 2: Role of Endothelin System in Health:
1. Vascular Tone Regulation: Endothelin is a potent vasoconstrictor and helps regulate blood pressure by influencing vascular smooth muscle tone.
2. Cell Growth and Repair: ET-1 promotes cell proliferation and fibrosis, which is essential in wound healing but can be detrimental in excess.
3. Renal Function Regulation: Endothelin plays a role in kidney function by regulating glomerular filtration, renal blood flow, and sodium handling in the kidneys.
Step 3: Role of Endothelin in Kidney Diseases:
1. Chronic Kidney Disease (CKD): Elevated endothelin levels are often found in CKD, contributing to vasoconstriction and glomerulosclerosis, which worsen kidney function.
2. Hypertension: Endothelin contributes to the pathogenesis of hypertension by promoting vasoconstriction and fluid retention.
3. Diabetic Nephropathy: Endothelin’s role in glomerular injury and fibrosis makes it a key player in diabetic nephropathy, contributing to the progression of renal damage. Quick Tip: The endothelin system is critical in maintaining vascular tone and kidney function, but its dysregulation plays a role in various kidney diseases.
Role of endothelin receptor antagonists in various kidney diseases.
View Solution
Step 1: Mechanism of Endothelin Receptor Antagonists (ERAs):
Endothelin receptor antagonists (ERAs) are a class of drugs that block the effects of endothelin by inhibiting its binding to the ET-A and ET-B receptors. By blocking ET-1, ERAs help reverse the vasoconstrictive and proliferative effects of endothelin.
Step 2: Role of ERAs in Kidney Diseases:
1. Chronic Kidney Disease (CKD): In CKD, ERAs help reduce glomerulosclerosis, improve renal blood flow, and decrease proteinuria by inhibiting the harmful effects of endothelin.
2. Hypertension: ERAs are useful in treating hypertension associated with kidney diseases, as they help reduce systemic vascular resistance and lower blood pressure.
3. Diabetic Nephropathy: In diabetic nephropathy, ERAs help protect against glomerular damage and fibrosis, potentially slowing the progression of renal dysfunction.
4. Polycystic Kidney Disease (PKD): ERAs have shown promise in reducing cyst growth and improving kidney function in animal models of PKD, though more clinical research is needed.
Step 3: Clinical Use and Considerations:
1. Clinical Trials: ERAs like bosentan, ambrisentan, and macitentan have shown efficacy in clinical trials for conditions like pulmonary hypertension, with potential benefits in kidney disease treatment.
2. Side Effects: The use of ERAs is associated with side effects like liver toxicity, anemia, and fluid retention, which need to be monitored during treatment.
3. Combination Therapy: ERAs may be used in combination with other antihypertensive or disease-modifying agents to improve renal outcomes in patients with progressive kidney disease. Quick Tip: Endothelin receptor antagonists offer a promising therapeutic approach in various kidney diseases, but careful monitoring for side effects is essential.




Comments