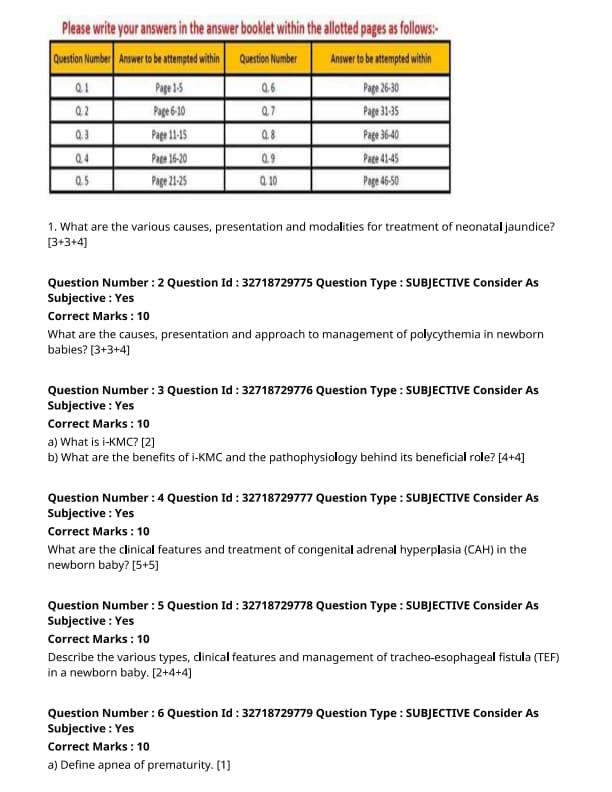
NEET SS 2024 DrNB Neonatology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Neonatology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Neonatology Paper 3 Question Paper | Check Solutions |

What are the various causes, presentation, and modalities for treatment of neonatal jaundice?
View Solution
Neonatal jaundice is a common condition in newborns, characterized by a yellowish discoloration of the skin and sclera due to an elevated level of bilirubin in the blood. It is important to identify the cause, monitor the severity, and provide appropriate treatment.
Step 1: Causes of Neonatal Jaundice:
1. Physiological Jaundice:
- Occurs in healthy newborns, typically after the first 24 hours of life. It is due to the immaturity of the liver's ability to process bilirubin.
- Common in premature infants as they have lower hepatic enzyme activity and slower elimination of bilirubin.
2. Pathological Jaundice:
- Hemolytic Disorders: Conditions like Rh incompatibility or ABO incompatibility can cause increased red blood cell breakdown, leading to higher bilirubin levels.
- G6PD Deficiency: Glucose-6-phosphate dehydrogenase deficiency can cause hemolysis, leading to jaundice.
- Infections: Infections like sepsis or TORCH infections (toxoplasmosis, rubella, cytomegalovirus, herpes) can cause jaundice.
- Biliary Atresia: A condition in which there is obstruction of the bile ducts, causing conjugated hyperbilirubinemia and jaundice.
3. Breastfeeding Jaundice:
- Caused by insufficient breastfeeding, leading to dehydration and a buildup of unconjugated bilirubin. Common in the first week of life.
Step 2: Presentation of Neonatal Jaundice:
1. Timing of Onset:
- Physiological Jaundice: Typically appears after the first 24 hours and resolves within 1-2 weeks in full-term infants.
- Pathological Jaundice: Appears within the first 24 hours or persists for longer than usual. This requires further investigation.
2. Clinical Features:
- Yellowing of the Skin and Sclera: The hallmark of jaundice. The severity is assessed by examining the extent of yellowing, starting from the face and progressing downward.
- Lethargy, Poor Feeding, and Vomiting: These can be signs of severe jaundice or an underlying illness.
- Dark Urine and Pale Stools: In cases of conjugated hyperbilirubinemia, such as biliary atresia, these symptoms can be present.
Step 3: Modalities for Treatment of Neonatal Jaundice:
1. Phototherapy:
- The most common treatment for jaundice. Blue light helps convert unconjugated bilirubin into a more water-soluble form that can be excreted in the urine.
- The baby is placed under phototherapy lamps or a light-emitting pad, ensuring that the skin is exposed to light.
2. Exchange Transfusion:
- Used in severe cases of jaundice, particularly when bilirubin levels are high enough to cause risk of kernicterus. It involves removing a portion of the infant's blood and replacing it with donor blood to quickly reduce bilirubin levels.
3. Intravenous Immunoglobulin (IVIG):
- Used in cases of hemolytic jaundice caused by Rh or ABO incompatibility to reduce the level of hemolysis and the associated bilirubin production.
4. Treatment of Underlying Causes:
- If jaundice is caused by an infection or metabolic disorder, specific treatment (e.g., antibiotics for infection or enzyme replacement for G6PD deficiency) will be necessary.
- In cases of biliary atresia, surgical interventions such as a Kasai procedure may be required to improve bile flow.
5. Improved Feeding:
- Ensuring that the infant is well-fed can help prevent breastfeeding jaundice by improving hydration and increasing bowel movements to promote the elimination of bilirubin. Quick Tip: Timely diagnosis and treatment of neonatal jaundice are crucial to prevent complications such as kernicterus, especially in severe cases. Phototherapy is effective in most cases, but more aggressive treatment may be needed in severe forms.
What are the causes, presentation, and approach to management of polycythemia in newborn babies?
View Solution
Polycythemia in newborns refers to an increase in the number of red blood cells, which can lead to hyperviscosity of the blood. This condition can present with various clinical symptoms and requires appropriate management.
Step 1: Causes of Polycythemia in Newborns:
1. Increased Erythropoiesis:
- Intrauterine Hypoxia: Conditions like maternal smoking, placental insufficiency, or living at high altitudes can lead to fetal hypoxia, stimulating erythropoiesis.
- Twin-Twin Transfusion Syndrome: This condition results in unequal blood volume distribution between twins, leading to polycythemia in the recipient twin.
- Delayed Clamping of the Umbilical Cord: This practice can lead to increased blood volume in the newborn, resulting in polycythemia.
2. Dehydration:
- Reduced Fluid Intake: Dehydration due to poor feeding or excessive fluid loss may lead to hemoconcentration, which mimics polycythemia.
3. Genetic Disorders:
- Familial Polycythemia: In rare cases, polycythemia is due to genetic mutations that result in increased production of erythropoietin.
Step 2: Presentation of Polycythemia in Newborns:
1. Clinical Symptoms:
- Cyanosis and Respiratory Distress: High red blood cell concentrations may cause poor oxygen delivery to tissues, leading to cyanosis.
- Poor Feeding and Lethargy: Increased blood viscosity can impair circulation and oxygenation, causing the infant to be lethargic and have difficulty feeding.
- Jaundice: Increased red blood cell turnover can lead to hyperbilirubinemia, resulting in jaundice.
2. Physical Findings:
- Plethora (Redness of the Skin): The infant may appear unusually red, especially on the face and upper body, due to the increased number of red blood cells.
- Abdominal Distension: In severe cases, splenomegaly or hepatomegaly may occur due to the increased workload of the liver and spleen in filtering excess red blood cells.
Step 3: Management of Polycythemia in Newborns:
1. Initial Assessment:
- Blood Tests: Confirm polycythemia with hematocrit levels greater than 65%. A complete blood count (CBC) and arterial blood gases should be performed to assess the severity of the condition.
- Hydration Status: Assess the infant’s hydration status to rule out dehydration as the cause of apparent polycythemia.
2. Management Strategies:
- Partial Exchange Transfusion: This is the primary treatment for symptomatic polycythemia. It helps to reduce the red blood cell mass and improve blood viscosity.
- Supportive Care: In cases of mild polycythemia without symptoms, supportive care with hydration and monitoring may suffice.
- Treating Underlying Conditions: If the polycythemia is secondary to underlying conditions such as intrauterine hypoxia or twin-twin transfusion syndrome, addressing those conditions is essential to prevent further complications.
3. Follow-up and Prevention:
- Monitoring: Frequent follow-up is necessary to monitor for complications like jaundice, respiratory distress, and feeding difficulties.
- Prevention: Delayed umbilical cord clamping should be carefully managed to avoid excessive blood volume in the newborn, and maternal conditions like smoking should be addressed to prevent intrauterine hypoxia. Quick Tip: Polycythemia in newborns should be managed based on severity, with partial exchange transfusion for symptomatic cases, and monitoring for complications like jaundice and respiratory distress.
What is i-KMC?
View Solution
i-KMC (Individualized Kangaroo Mother Care) is an evolved form of the traditional Kangaroo Mother Care (KMC), which is a method of care for premature or low-birth-weight infants. It involves skin-to-skin contact between the infant and the caregiver (usually the mother), which provides warmth, promotes bonding, and improves health outcomes for the infant.
Step 1: Definition of i-KMC:
1. Individualized Care: i-KMC refers to the personalized approach to Kangaroo Mother Care, where the care plan is tailored to the individual needs of both the infant and the caregiver. It goes beyond the basic concept of skin-to-skin contact and includes the provision of other elements of care based on the infant's medical condition, such as breastfeeding, respiratory support, and sensory stimulation.
2. Flexible Approach: Unlike the rigid schedule of traditional KMC, i-KMC allows for flexibility in the duration and frequency of contact, based on the specific needs of the infant and the family's situation. Quick Tip: i-KMC is an individualized and flexible approach to Kangaroo Mother Care, focused on optimizing care based on the unique needs of premature infants.
What are the benefits of i-KMC and the pathophysiology behind its beneficial role?
View Solution
i-KMC (Individualized Kangaroo Mother Care) provides several benefits to premature and low-birth-weight infants. The approach promotes optimal growth, development, and well-being through physical closeness and tailored care, while the pathophysiological mechanisms behind its benefits are related to the physiological effects of skin-to-skin contact and early parent-child bonding.
Step 1: Benefits of i-KMC:
1. Thermoregulation: i-KMC helps regulate the infant’s body temperature through skin-to-skin contact, reducing the risk of hypothermia, which is common in preterm infants. The mother's body provides a natural source of warmth, helping to maintain optimal thermal conditions.
2. Improved Breastfeeding: Skin-to-skin contact promotes successful breastfeeding by enhancing the infant's sucking reflex and encouraging the production of breast milk, which is crucial for the infant's immune function and growth.
3. Neurological Development: i-KMC stimulates the infant’s nervous system, promoting brain development and cognitive function. It helps with sensory development by providing physical stimulation and interaction with the caregiver.
4. Reduced Mortality and Morbidity: Studies show that i-KMC reduces the risk of infections, improves oxygenation, and lowers the incidence of apnea and bradycardia in preterm infants. It also decreases the chances of neurological impairments and other long-term developmental issues.
Step 2: Pathophysiology Behind the Beneficial Role:
1. Skin-to-Skin Contact and Hormonal Regulation: Skin-to-skin contact triggers the release of hormones like oxytocin, which facilitates milk production and enhances maternal bonding. Oxytocin also reduces stress and promotes relaxation, benefiting both the infant and the caregiver.
2. Cardiovascular and Respiratory Stabilization: i-KMC helps regulate the infant's cardiovascular system by improving heart rate and blood pressure. The close contact stimulates the infant’s respiratory system, leading to improved oxygenation and reduced episodes of apnea.
3. Immune System Enhancement: The physical closeness to the mother exposes the infant to beneficial microbes, helping to establish a healthy microbiome, which is essential for the development of the infant's immune system. This reduces the risk of infections and boosts overall health.
4. Reduced Stress Response: The warmth and comfort provided by i-KMC reduce the stress response in infants, lowering cortisol levels and promoting overall well-being. Quick Tip: i-KMC provides numerous health benefits to preterm infants by regulating their temperature, promoting development, enhancing immune function, and reducing the risk of complications.
What are the clinical features and treatment of congenital adrenal hyperplasia (CAH) in the newborn baby?
View Solution
Congenital adrenal hyperplasia (CAH) is a group of inherited disorders that lead to deficiencies in enzymes required for adrenal steroidogenesis. The most common form is 21-hydroxylase deficiency, which causes decreased cortisol and aldosterone production, and an increase in androgen production.
Step 1: Clinical Features of CAH in Newborns:
1. Salt Wasting (Classic CAH):
- This is the most severe form of CAH. Affected newborns cannot produce aldosterone, leading to salt wasting, dehydration, and hyperkalemia. This results in symptoms such as vomiting, poor feeding, weight loss, lethargy, and hypovolemic shock. If not treated, this condition can lead to death in the first weeks of life.
2. Ambiguous Genitalia (Classic CAH):
- In female infants, excessive androgen production leads to virilization of the external genitalia, causing clitoromegaly and labial fusion, which can be mistaken for male genitalia. In male infants, virilization is typically less noticeable at birth, but early signs of puberty may develop.
3. Non-Salt Wasting (Simple Virilizing CAH):
- In this less severe form of CAH, there is sufficient aldosterone production, so salt-wasting is not a concern. However, excessive androgen production still leads to virilization of female genitalia. These infants may also develop early signs of puberty.
4. Cortisol Deficiency:
- Infants with CAH may present with cortisol deficiency, resulting in hypoglycemia, lethargy, and poor feeding. This deficiency can further contribute to dehydration and weight loss.
Step 2: Treatment of CAH in Newborns:
1. Glucocorticoid Replacement:
- The cornerstone of treatment for CAH is the replacement of cortisol with glucocorticoids such as hydrocortisone. The dose is carefully adjusted to both suppress the excessive androgen production and ensure normal growth and development.
2. Mineralocorticoid Replacement (for Salt-Wasting CAH):
- For salt-wasting forms of CAH, fludrocortisone is administered to replace aldosterone and help the body retain sodium, thus preventing dehydration and hypovolemia. This is essential in the early life of the infant.
3. Surgical Management (for Ambiguous Genitalia):
- Female infants with ambiguous genitalia may require reconstructive surgery to normalize the appearance of the external genitalia. This is usually done later in infancy or early childhood, depending on the severity of the genital virilization.
4. Monitoring and Support:
- Regular monitoring of electrolytes, growth, and development is crucial. In the early days of life, close monitoring of fluid and electrolyte balance is required, especially in salt-wasting forms.
- Lifelong glucocorticoid therapy is required, and the dosage may need to be adjusted during times of stress (e.g., infections or surgeries). Salt and fluid intake should be monitored, particularly in the first few months. Quick Tip: Early diagnosis and treatment of CAH are essential to prevent life-threatening conditions such as adrenal crisis. Lifelong management is needed to maintain normal growth and prevent complications.
Describe the various types, clinical features and management of tracheo-esophageal fistula (TEF) in a newborn baby.
View Solution
Step 1: Types of Tracheo-Esophageal Fistula (TEF):
TEF is a congenital condition where there is an abnormal connection between the trachea and esophagus. The most common types of TEF are classified by the Gross classification:
1. Type A (isolated esophageal atresia): This is the most common type where there is no connection between the upper and lower segments of the esophagus. There is no TEF.
2. Type B: This type involves a connection between the lower esophagus and the trachea, with an upper esophageal pouch.
3. Type C (most common): A fistula between the trachea and lower esophagus, with an upper esophageal pouch.
4. Type D: A double fistula between the trachea and both upper and lower esophagus.
5. Type E (H-type): This type involves an isolated fistula between the trachea and the esophagus, with both segments of the esophagus being intact.
Step 2: Clinical Features of TEF in Newborns:
The clinical presentation of TEF can vary depending on the type of fistula. Common signs include:
1. Excessive Drooling: The newborn may present with excessive salivation, which is a result of the inability to swallow saliva.
2. Coughing or Choking: The baby may cough or choke, especially during feeding, as milk or formula can enter the trachea through the fistula.
3. Respiratory Distress: Difficulty breathing due to aspiration and aspiration pneumonia is common.
4. Failure to Thrive: In cases with a significant esophageal defect, feeding difficulties lead to inadequate nutrition and growth.
5. Abdominal Distention: This can be a result of air entering the stomach from the trachea due to the fistula.
Step 3: Management of TEF in Newborns:
1. Preoperative Care:
- Nasogastric Tube (NGT): An NGT is often placed to decompress the stomach and prevent aspiration.
- Respiratory Support: Babies may need oxygen therapy or mechanical ventilation to manage respiratory distress.
- Antibiotics: If pneumonia is present, broad-spectrum antibiotics are administered.
2. Surgical Repair:
- TEF Repair: The preferred treatment is surgical closure of the fistula, typically done through thoracotomy.
- Esophageal Reconstruction: In cases where there is esophageal atresia, a primary anastomosis may be performed, or a staged procedure may be required to connect the upper and lower segments of the esophagus.
3. Postoperative Care:
- Feeding and Nutrition: After surgery, enteral feeding is usually introduced slowly, with parenteral nutrition if necessary.
- Monitoring: Continuous monitoring for complications such as leakage, infection, or stricture formation is crucial.
Quick Tip: Early diagnosis and surgical repair are key to preventing long-term complications of TEF, including aspiration pneumonia, nutritional deficiencies, and esophageal stricture.
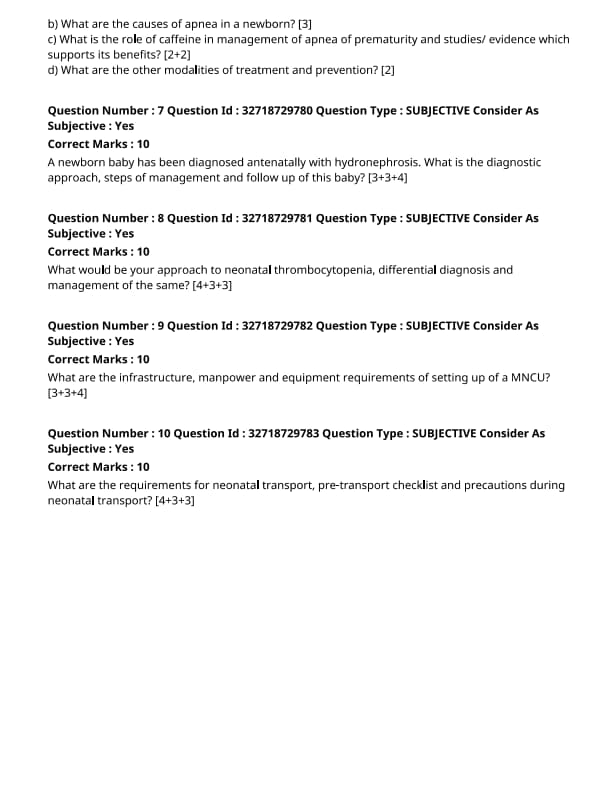
Define apnea of prematurity.
View Solution
Apnea of prematurity (AOP) is the cessation of breathing for more than 20 seconds due to immature respiratory control mechanisms in preterm infants, often accompanied by bradycardia and oxygen desaturation. Quick Tip: Apnea is more common in infants born before 28 weeks of gestation and usually improves as the infant matures.
What are the causes of apnea in a newborn?
View Solution
The causes of apnea in a newborn can be broadly classified into three categories: respiratory, central, and metabolic causes.
Step 1: Respiratory Causes:
1. Respiratory Distress Syndrome (RDS): Insufficient surfactant production in premature infants can cause lung collapse and inadequate oxygenation, leading to apnea.
2. Infections: Respiratory infections, such as sepsis or pneumonia, can cause apnea by affecting the respiratory system.
Step 2: Central Causes:
1. Immaturity of Respiratory Centers: Premature infants have underdeveloped brainstem respiratory centers, leading to irregular breathing patterns.
2. Neurological Disorders: Conditions such as intraventricular hemorrhage or brain malformations may impair respiratory regulation.
Step 3: Metabolic Causes:
1. Hypoglycemia: Low blood sugar levels can result in apnea, especially in premature or sick infants.
2. Electrolyte Imbalances: Abnormal levels of sodium, calcium, or potassium can cause irregular respiratory control. Quick Tip: Identifying and addressing the underlying cause of apnea is essential for effective treatment and management.
What is the role of caffeine in management of apnea of prematurity and studies/evidence which supports its benefits?
View Solution
Caffeine is a central respiratory stimulant commonly used to treat apnea of prematurity by stimulating the brainstem and improving the respiratory drive.
Step 1: Mechanism of Action:
Caffeine works by antagonizing adenosine receptors in the brainstem, which promotes respiratory drive and improves respiratory patterns, reducing episodes of apnea.
Step 2: Evidence and Studies:
1. Effectiveness in Reducing Apnea Episodes: Several randomized controlled trials have shown that caffeine significantly reduces the frequency and severity of apnea episodes in premature infants.
2. Safety Profile: Caffeine has a favorable safety profile compared to other respiratory stimulants, with few adverse effects such as tachycardia or gastrointestinal irritation.
Step 3: Long-term Benefits:
1. Neurodevelopmental Outcome: Studies suggest that caffeine therapy may improve neurodevelopmental outcomes in extremely low birth weight infants by reducing the risk of long-term developmental delays.
2. Reduced Need for Mechanical Ventilation: Caffeine reduces the need for invasive mechanical ventilation, leading to shorter durations of mechanical ventilation and hospitalization. Quick Tip: Caffeine therapy is commonly used in neonatal care for apnea of prematurity, and its use has been widely supported by clinical evidence.
What are the other modalities of treatment and prevention?
View Solution
In addition to caffeine therapy, several other modalities are used for the treatment and prevention of apnea of prematurity.
Step 1: Respiratory Support:
1. Continuous Positive Airway Pressure (CPAP): CPAP is used to maintain airway patency and prevent atelectasis, reducing the incidence of apnea.
2. Mechanical Ventilation: In severe cases of apnea, mechanical ventilation may be required to support the infant's respiratory function until the infant's respiratory control improves.
Step 2: Prevention Strategies:
1. Antenatal Steroids: Administration of corticosteroids to mothers at risk of preterm labor helps accelerate fetal lung maturation, reducing the risk of RDS and subsequent apnea.
2. Methylxanthine Therapy: In some cases, medications like theophylline may be used as an alternative to caffeine, though caffeine is preferred due to its better safety profile. Quick Tip: A combination of respiratory support, caffeine, and preventive strategies is typically used to manage and reduce the occurrence of apnea of prematurity in preterm infants.
A newborn baby has been diagnosed antenatally with hydronephrosis. What is the diagnostic approach, steps of management, and follow-up of this baby?
View Solution
Hydronephrosis is a common condition detected during routine antenatal ultrasounds. It refers to the dilation of the renal pelvis and calyces due to impaired urine flow. Proper diagnostic evaluation, management, and follow-up are critical to prevent complications such as renal damage.
Step 1: Diagnostic Approach:
1. Confirmatory Ultrasound:
- A postnatal ultrasound is the first step to confirm the diagnosis and assess the severity of hydronephrosis. The degree of hydronephrosis is classified based on the anteroposterior renal pelvic diameter (APD).
- If APD is greater than 7-10 mm, further evaluation is warranted.
2. Voiding Cystourethrogram (VCUG):
- If vesicoureteral reflux (VUR) is suspected (a common cause of hydronephrosis), a VCUG is done to assess the bladder and urethra for reflux of urine from the bladder back into the kidneys.
3. Magnetic Resonance Urography (MRU):
- In cases where the etiology is unclear or when anatomical anomalies like obstruction or pyeloureteral junction (PUJ) stenosis are suspected, MRU may provide more detailed imaging.
4. Renal Scintigraphy:
- In some cases, a renal scan with technetium-99m dimercaptosuccinic acid (DMSA) or mercaptoacetyltriglycine (MAG3) is used to assess renal function and perfusion.
Step 2: Management:
1. Observation:
- In cases of mild hydronephrosis, particularly if there is no evidence of infection or other complications, conservative management with regular monitoring via ultrasound may be appropriate.
- Follow-up ultrasounds every 6-12 weeks are recommended to monitor the progression.
2. Medical Treatment:
- If urinary tract infection (UTI) is suspected or confirmed, appropriate antibiotic treatment should be initiated. Antibiotic prophylaxis is often started for infants with significant hydronephrosis or VUR to prevent UTIs.
3. Surgical Treatment:
- Surgical intervention may be required for significant hydronephrosis caused by obstructive uropathy (e.g., PUJ obstruction or posterior urethral valves).
- Procedures may include pyeloplasty for PUJ obstruction or valve ablation for posterior urethral valves.
4. Management of VUR:
- For infants with significant VUR, surgical correction may be necessary, although many mild cases resolve spontaneously. In some cases, endoscopic injection of bulking agents is an option.
Step 3: Follow-up:
1. Regular Ultrasound Monitoring:
- Follow-up ultrasounds should be scheduled to monitor the resolution of hydronephrosis or any progression of kidney damage.
- Monitoring is especially important for the first 2 years of life as the renal system matures.
2. Urological Consultation:
- Infants with moderate to severe hydronephrosis, especially those with VUR, should be referred to a pediatric urologist for further management.
3. Renal Function Monitoring:
- Regular renal function tests (creatinine, urea) and blood pressure checks should be done to assess kidney function, especially if surgery or significant hydronephrosis is present.
4. Long-Term Follow-Up:
- Even after successful treatment, some children may need long-term follow-up into childhood to ensure normal renal function and prevent complications like hypertension or renal insufficiency.
Quick Tip: Timely intervention and regular follow-up are crucial in managing hydronephrosis in newborns to prevent long-term renal damage.
What are the infrastructure, manpower and equipment requirements of setting up of a MNCU?
View Solution
Setting up a Maternal and Neonatal Care Unit (MNCU) requires careful planning to ensure the safety and well-being of both mothers and newborns. The key factors to consider include infrastructure, manpower, and equipment requirements.
Step 1: Infrastructure Requirements:
1. Space: The MNCU should be located in a spacious and easily accessible area, ideally near the labor and delivery rooms. It should have separate areas for maternity beds, neonatal care, and staff.
2. Environmental Control: Proper ventilation, temperature control, and lighting are essential for maintaining a sterile and comfortable environment. The unit should be equipped with air conditioning and humidity control systems.
3. Sanitation: The unit must have strict infection control measures in place, including hand hygiene stations, sterilization areas, and waste management systems.
Step 2: Manpower Requirements:
1. Doctors and Specialists: An experienced obstetrician and neonatologist should be available round the clock to manage high-risk deliveries and neonatal care.
2. Nurses: The unit should have trained and skilled nurses specializing in maternal and neonatal care, with adequate staff-to-patient ratios. Nurses should be trained in neonatal resuscitation and other life-saving techniques.
3. Support Staff: Other staff members, including laboratory technicians, radiologists, and physiotherapists, should be available to support the medical and nursing staff.
Step 3: Equipment Requirements:
1. Maternal Care Equipment: Essential equipment includes delivery beds, fetal monitors, intravenous infusion pumps, and blood pressure monitors.
2. Neonatal Care Equipment: Neonatal incubators, radiant warmers, oxygen supply systems, neonatal ventilators, and phototherapy units for jaundiced babies are crucial.
3. Emergency and Resuscitation Equipment: The MNCU should be equipped with neonatal resuscitation equipment, including a neonatal resuscitation bag, laryngoscopes, endotracheal tubes, and suction devices.
4. Diagnostic Equipment: Ultrasound machines, blood gas analyzers, and diagnostic labs should be available for quick assessments and to monitor the health of the mother and infant. Quick Tip: Proper infrastructure, trained manpower, and state-of-the-art equipment are vital for the effective functioning of an MNCU, ensuring the health and safety of both mother and baby.
What are the requirements for neonatal transport, pre-transport checklist and precautions during neonatal transport?
View Solution
Step 1: Requirements for Neonatal Transport:
1. Transport Equipment: The transport team must ensure that all necessary equipment is available, including a neonatal transport incubator, ventilator, oxygen supply, monitoring devices (e.g., pulse oximeter, ECG), and infusion pumps.
2. Skilled Personnel: The transport team should include a neonatologist, nurse, and respiratory therapist who are experienced in managing critically ill neonates.
3. Stabilization of the Neonate: Before transport, the neonate must be properly stabilized, including management of airway, breathing, circulation, and temperature regulation.
4. Documentation and Communication: Complete medical records, including the neonate’s condition and medical history, should be provided to the receiving team. Clear communication must be established with the receiving hospital.
Step 2: Pre-Transport Checklist:
1. Vital Signs Monitoring: Confirm that vital signs, including heart rate, blood pressure, respiratory rate, and temperature, are within stable limits.
2. Oxygenation and Ventilation: Ensure appropriate oxygen delivery and ventilation support, either via mechanical ventilation or non-invasive methods, depending on the neonate’s condition.
3. Intravenous Access: Secure reliable intravenous (IV) access for administering fluids, medications, and nutrients.
4. Medications and Emergency Drugs: Ensure that all necessary medications, including antibiotics, sedatives, or emergency drugs, are prepared and available during transport.
Step 3: Precautions During Neonatal Transport:
1. Temperature Control: Maintain the neonate’s body temperature within the normal range, using an incubator or appropriate heating mechanisms to prevent hypothermia or hyperthermia.
2. Continuous Monitoring: Throughout transport, continuous monitoring of vital signs, oxygen saturation, and ventilation should be done. Adjustments to support may be needed based on the neonate's condition.
3. Safe Transport Practices: Secure the neonate in the transport incubator to prevent injury or discomfort. Be mindful of the road conditions and avoid rapid movements during transport to prevent any additional stress or injury to the neonate. Quick Tip: Proper planning, stabilization, and monitoring are key to ensuring the safety and well-being of the neonate during transport.




Comments