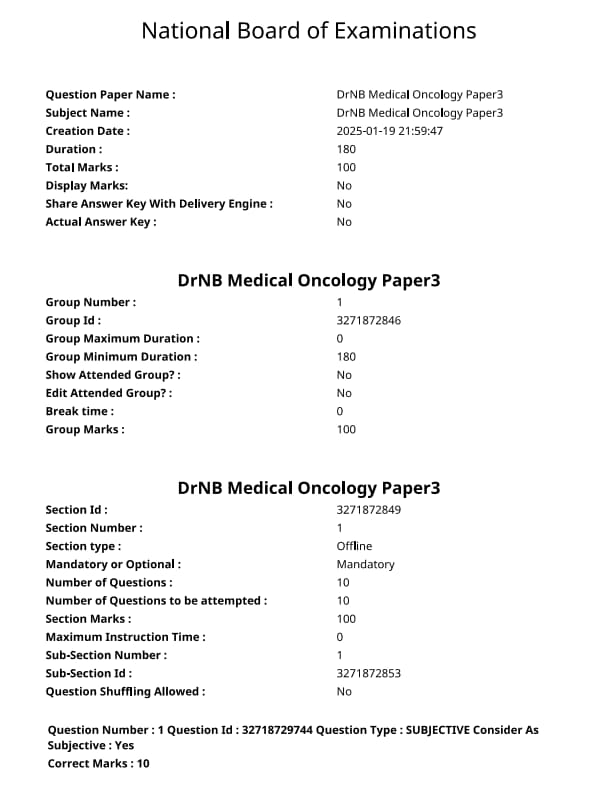
NEET SS 2024 DrNB Medical Oncology Paper 3 Question Paper with Solutions PDF is available for download. NEET SS 2024 exam is conducted by the National Board of Examinations in Medical Sciences (NBEMS). NEET SS 2024 question paper consists of 10 questions to be attempted in 3 hours. The paper is divided into broad-specialty topics (40%) and super-specialty topics (60%).
You can download NEET SS 2024 question paper with answer key and solutions PDF using the links given below.
NEET SS 2024 DrNB Medical Oncology Paper 3 Question Paper with Solutions
| NEET SS 2024 DrNB Medical Oncology Paper 3 Question Paper | Check Solutions |

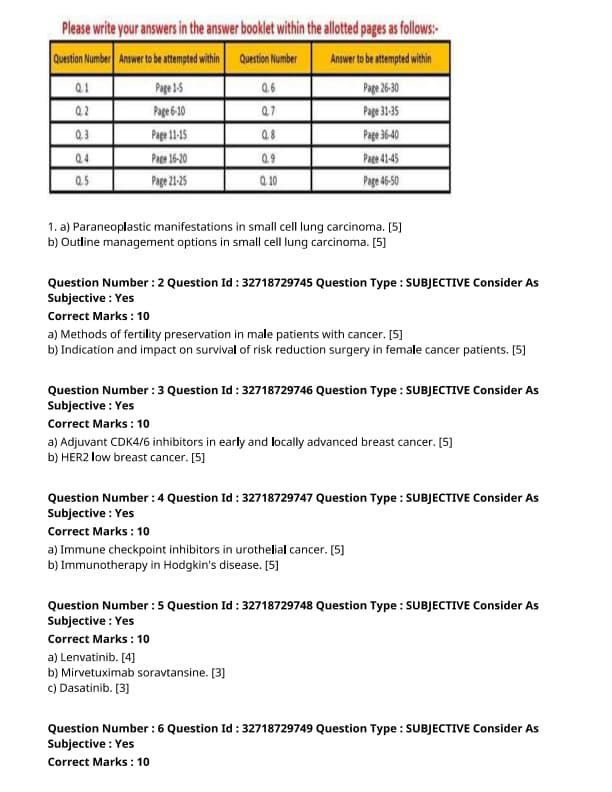
Paraneoplastic manifestations in small cell lung carcinoma.
View Solution
Small cell lung carcinoma (SCLC) is an aggressive form of lung cancer that can present with various paraneoplastic manifestations. These manifestations occur due to the ectopic production of hormones or hormone-like substances by tumor cells. Paraneoplastic syndromes in SCLC are often associated with poor prognosis.
Step 1: Common Paraneoplastic Manifestations:
1. SIADH (Syndrome of Inappropriate Antidiuretic Hormone Secretion): This is the most common paraneoplastic syndrome in SCLC. It leads to hyponatremia due to excessive secretion of ADH.
2. Cushing’s Syndrome: Occurs due to ectopic production of ACTH (Adrenocorticotropic hormone), which stimulates cortisol release, causing symptoms like weight gain, hypertension, and hyperglycemia.
3. Lambert-Eaton Myasthenic Syndrome (LEMS): Characterized by muscle weakness and is caused by autoantibodies against presynaptic voltage-gated calcium channels.
4. Hypercalcemia: May occur due to the production of parathyroid hormone-related protein (PTHrP), which increases calcium levels.
Step 2: Diagnostic Approach:
1. Serum and urine tests for sodium and cortisol levels to identify SIADH and Cushing's syndrome.
2. Antibody tests for Lambert-Eaton myasthenic syndrome.
3. Measurement of PTHrP and calcium levels for hypercalcemia. Quick Tip: Early recognition of paraneoplastic syndromes in small cell lung carcinoma can guide treatment decisions and improve patient outcomes.
Outline management options in small cell lung carcinoma.
View Solution
Management of small cell lung carcinoma (SCLC) is primarily focused on controlling the tumor, managing symptoms, and improving quality of life. Treatment strategies often include a combination of chemotherapy, radiation, and in some cases, surgery.
Step 1: Chemotherapy:
1. First-line treatment: The mainstay of treatment is chemotherapy, typically with a combination of etoposide and platinum-based agents (cisplatin or carboplatin). This combination has shown to improve survival in extensive-stage SCLC.
2. Chemotherapy in limited-stage disease: Chemotherapy is combined with chest radiation to increase survival chances. Prophylactic cranial irradiation (PCI) is recommended to prevent brain metastasis.
Step 2: Radiation Therapy:
1. Thoracic radiation: In limited-stage disease, thoracic radiation is used along with chemotherapy to treat localized tumors.
2. Prophylactic cranial irradiation (PCI): PCI is used to reduce the risk of brain metastasis in patients who respond well to chemotherapy.
Step 3: Immunotherapy:
1. Recent advances: Immune checkpoint inhibitors, such as pembrolizumab or atezolizumab, have shown promise in treating SCLC, especially when used in combination with chemotherapy for extensive-stage disease.
Step 4: Supportive Care:
1. Symptom management: Management of paraneoplastic syndromes, pain control, and addressing side effects from chemotherapy are important aspects of supportive care. Quick Tip: Combination chemotherapy, radiation, and immunotherapy offer the best outcomes for small cell lung carcinoma, but early diagnosis and treatment are key to improving prognosis.
Methods of fertility preservation in male patients with cancer.
View Solution
Fertility preservation is an important consideration for male cancer patients, especially those undergoing treatments like chemotherapy or radiation that can impair fertility. Several methods are available to help preserve fertility:
Step 1: Sperm Banking:
This is the most commonly used method where sperm is collected and frozen before cancer treatment begins. The sperm can later be used for assisted reproductive technologies such as in vitro fertilization (IVF).
Step 2: Testicular Sperm Extraction (TESE):
In cases where sperm production is impaired, testicular sperm extraction may be performed. This involves surgically retrieving sperm directly from the testicles, which can then be used in IVF or intracytoplasmic sperm injection (ICSI).
Step 3: Hormonal Therapy:
In some cases, hormonal therapy, such as the use of testosterone, may be used to protect spermatogenesis (sperm production) during cancer treatment. Quick Tip: Sperm banking is the most common and effective method for fertility preservation in male cancer patients, but options like TESE can be used if sperm count is low or absent.
Indication and impact on survival of risk reduction surgery in female cancer patients.
View Solution
Risk reduction surgery is commonly considered in female cancer patients who are at high risk of developing cancer due to genetic predisposition, such as BRCA1 or BRCA2 mutations. This surgical approach aims to reduce the risk of developing certain cancers, such as breast or ovarian cancer, in at-risk individuals.
Step 1: Indication for Surgery:
1. Genetic Predisposition: Women with BRCA mutations are at significantly higher risk for breast and ovarian cancers. Prophylactic surgeries, such as mastectomy (breast removal) or oophorectomy (ovary removal), may be recommended.
2. Family History: A strong family history of breast or ovarian cancer can also indicate the need for risk-reduction surgery, especially if the patient carries genetic mutations that increase their risk.
Step 2: Impact on Survival:
1. Improved Survival Rates: Prophylactic mastectomies and oophorectomies significantly reduce the risk of cancer development and improve overall survival rates by preventing cancer in high-risk individuals.
2. Psychosocial Considerations: While these surgeries reduce the risk of cancer, they may also have psychological and hormonal effects, such as early menopause, which need to be carefully managed. Quick Tip: Risk reduction surgery, such as mastectomy and oophorectomy, has been shown to significantly reduce cancer risk and improve survival in women with genetic predispositions like BRCA mutations.
Adjuvant CDK4/6 inhibitors in early and locally advanced breast cancer.
View Solution
Adjuvant CDK4/6 inhibitors are a class of targeted therapy used in early and locally advanced breast cancer, particularly in hormone receptor-positive (HR+) cases. These inhibitors work by blocking the cyclin-dependent kinases 4 and 6, which are crucial for the cell cycle and tumor cell proliferation. By inhibiting these kinases, the treatment aims to reduce cancer cell growth and improve patient survival rates.
Step 1: Mechanism of Action:
CDK4/6 inhibitors work by preventing the phosphorylation of the retinoblastoma protein (Rb), leading to cell cycle arrest at the G1 phase. This stops the cancer cells from proliferating.
Step 2: Indications:
1. Early-stage HR+ breast cancer: CDK4/6 inhibitors are used in combination with hormonal therapies like aromatase inhibitors.
2. Locally advanced HR+ breast cancer: These inhibitors are also used in combination with chemotherapy to improve response rates.
Step 3: Side Effects:
1. Neutropenia: A common side effect, leading to an increased risk of infection.
2. Fatigue: Some patients may experience fatigue during treatment.
3. Gastrointestinal issues: Diarrhea is a frequent side effect that needs to be managed. Quick Tip: CDK4/6 inhibitors are effective in HR+ breast cancer, especially when used in combination with other therapies like hormonal treatments. Monitoring for side effects is important for patient management.
HER2 low breast cancer.
View Solution
HER2 low breast cancer refers to a subtype of breast cancer where there is a low expression of the HER2 protein. HER2 (Human Epidermal Growth Factor Receptor 2) is a protein that, when overexpressed, drives the growth of certain types of breast cancer. In HER2 low breast cancer, there is less HER2 expression, which may influence treatment strategies.
Step 1: Understanding HER2 Low Expression:
HER2 low cancers show some level of HER2 expression but not enough to be classified as HER2-positive. This category is distinct from HER2-negative breast cancer, where no HER2 overexpression is detected.
Step 2: Treatment Options for HER2 Low Cancer:
1. Targeted therapies: New therapies like trastuzumab deruxtecan are being investigated for their effectiveness in HER2 low breast cancer, showing promising results in clinical trials.
2. Chemotherapy: Traditional chemotherapy may be used in cases where HER2-targeted treatments are not effective.
Step 3: Prognosis and Challenges:
HER2 low breast cancer is still being studied, and treatment regimens continue to evolve. While patients with HER2 low cancers may have better outcomes than those with HER2-positive cancers, more research is needed to understand optimal treatment approaches and improve survival rates. Quick Tip: HER2 low breast cancer is a developing area of research, with new treatments showing potential. Understanding the molecular characteristics of these cancers is key to improving patient outcomes.
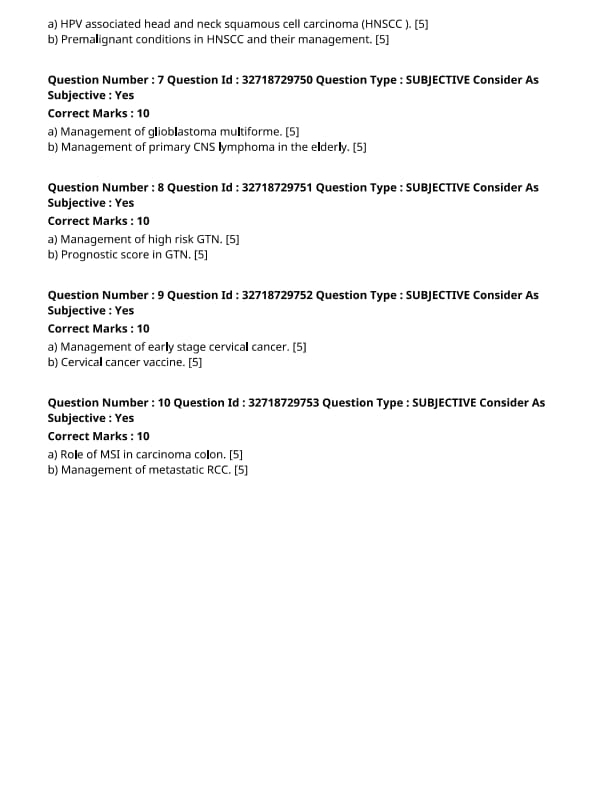
Immune checkpoint inhibitors in urothelial cancer.
View Solution
Immune checkpoint inhibitors (ICIs) are a class of cancer immunotherapies that have shown significant promise in the treatment of various cancers, including urothelial carcinoma. These therapies target immune checkpoints such as PD-1, PD-L1, and CTLA-4, which are regulatory molecules that cancer cells exploit to evade the immune system.
Step 1: Mechanism of Action:
1. PD-1/PD-L1 Inhibition: PD-1 is a checkpoint protein on immune cells, and PD-L1 is its ligand on cancer cells. When PD-L1 binds to PD-1, it inhibits T-cell activity, allowing cancer cells to escape immune surveillance. Inhibiting this interaction with drugs like pembrolizumab and nivolumab can restore immune function.
2. CTLA-4 Inhibition: CTLA-4 is another immune checkpoint that negatively regulates T-cell activation. Drugs like ipilimumab target this checkpoint to enhance T-cell responses against cancer cells.
Step 2: Clinical Use in Urothelial Cancer:
1. Approved Treatments: Several ICIs have been approved for urothelial carcinoma, including pembrolizumab and atezolizumab. These have shown efficacy in patients with advanced or metastatic disease who have failed prior chemotherapy.
2. Combination Therapies: Ongoing research is exploring the use of ICIs in combination with chemotherapy, targeted therapies, or other immune-modulating agents to improve response rates and overcome resistance mechanisms.
Step 3: Challenges and Future Directions:
1. Response Variability: Not all patients respond to ICIs, and there is a need to identify biomarkers that predict which patients will benefit the most.
2. Immune-Related Adverse Events (irAEs): ICIs can cause immune-related side effects, which can be severe and require careful management. Quick Tip: While immune checkpoint inhibitors offer promising results in urothelial cancer, their use is associated with challenges such as immune-related adverse events and variability in patient response.
Immunotherapy in Hodgkin's disease.
View Solution
Immunotherapy has become an essential treatment modality in Hodgkin’s disease, particularly for patients with relapsed or refractory disease. It involves using drugs that stimulate the immune system to recognize and attack cancer cells.
Step 1: Mechanism of Immunotherapy in Hodgkin's Disease:
1. Checkpoint Inhibition: PD-1 inhibitors like nivolumab and pembrolizumab have shown effectiveness in treating relapsed Hodgkin’s lymphoma. These drugs block the interaction between PD-1 on T-cells and PD-L1 on tumor cells, enhancing T-cell activation and anti-tumor immune responses.
2. Monoclonal Antibodies: Brentuximab vedotin is an antibody-drug conjugate targeting CD30, a protein expressed on Hodgkin’s lymphoma cells. It delivers a toxic agent directly to cancer cells, improving outcomes in patients who have failed conventional therapies.
Step 2: Clinical Use in Hodgkin’s Disease:
1. First-Line Treatment: Immunotherapy is often used after failure of traditional chemotherapy or stem cell transplants. It has shown effectiveness in improving progression-free survival in patients with refractory disease.
2. Combination Therapies: New studies are investigating combining immunotherapy with chemotherapy or other immune modulators to enhance treatment efficacy.
Step 3: Challenges and Future Directions:
1. Treatment Resistance: While many patients respond to immunotherapy, resistance remains a challenge, necessitating further research into combination therapies.
2. Adverse Effects: Immune-related adverse effects, including autoimmune reactions, can complicate treatment and require careful monitoring. Quick Tip: Immunotherapy, particularly with PD-1 inhibitors, has revolutionized the treatment of Hodgkin’s disease, especially in patients who do not respond to traditional therapies.
Lenvatinib.
View Solution
Lenvatinib is a tyrosine kinase inhibitor used primarily for the treatment of thyroid cancer and renal cell carcinoma. It inhibits multiple receptor tyrosine kinases involved in angiogenesis, including VEGFR1-3, FGFR1-4, PDGFRα, and KIT, which play critical roles in tumor cell growth and survival.
Step 1: Mechanism of Action:
Lenvatinib binds to and inhibits several receptor tyrosine kinases, blocking the signals that lead to angiogenesis, a critical process for tumor growth.
Step 2: Clinical Uses:
Lenvatinib is used for the treatment of advanced thyroid cancer, renal cell carcinoma, and hepatocellular carcinoma in certain patient populations.
Step 3: Dosage and Administration:
Lenvatinib is typically administered orally once a day, with the dose adjusted depending on the patient's response and tolerability. Quick Tip: Lenvatinib is commonly used in combination with other drugs such as everolimus to enhance its therapeutic effects.
Mirvetuximab soravtansine.
View Solution
Mirvetuximab soravtansine is an antibody-drug conjugate that targets the folate receptor alpha (FRα), which is overexpressed in certain types of cancer, particularly ovarian cancer. It consists of a monoclonal antibody linked to a cytotoxic agent, which is released into cancer cells upon binding to FRα.
Step 1: Mechanism of Action:
The antibody portion of Mirvetuximab soravtansine binds to FRα, and the cytotoxic drug is internalized into the cell. The drug then disrupts cellular processes, leading to cancer cell death.
Step 2: Clinical Uses:
Mirvetuximab soravtansine is being investigated in clinical trials for the treatment of ovarian cancer and other cancers expressing FRα.
Step 3: Dosage and Administration:
The recommended dosing schedule is determined by the clinical trial protocols, as Mirvetuximab soravtansine is still under investigation for certain indications. Quick Tip: Mirvetuximab soravtansine is an exciting new option in targeted cancer therapy, offering potential for specific tumor destruction with minimal side effects.
Dasatinib.
View Solution
Dasatinib is a multi-targeted kinase inhibitor primarily used in the treatment of chronic myelogenous leukemia (CML) and acute lymphoblastic leukemia (ALL). It targets several tyrosine kinases, including BCR-ABL, SRC family kinases, and others that are involved in cancer cell proliferation.
Step 1: Mechanism of Action:
Dasatinib inhibits BCR-ABL, the abnormal protein produced by the Philadelphia chromosome, and other kinases that are important for the survival and growth of leukemia cells.
Step 2: Clinical Uses:
Dasatinib is primarily used to treat Philadelphia chromosome-positive CML and ALL in patients who are resistant or intolerant to other therapies, such as imatinib.
Step 3: Dosage and Administration:
Dasatinib is taken orally, with the dose adjusted based on the patient's condition and treatment response. Quick Tip: Dasatinib is effective in patients with CML who have developed resistance to imatinib, providing a second-line treatment option.
Role of MSI in carcinoma colon.
View Solution
Microsatellite instability (MSI) is a condition of genetic hypermutability that occurs when the DNA mismatch repair (MMR) system is defective. In colon carcinoma, MSI plays a crucial role in tumorigenesis and is a marker for prognosis and therapy response.
Step 1: Mechanism of MSI in Colon Carcinoma:
MSI occurs when there are defects in the MMR system, leading to an accumulation of mutations in microsatellites, which are short, repetitive sequences of DNA. This can result in the activation of oncogenes or the inactivation of tumor suppressor genes.
Step 2: Clinical Implications:
MSI is often seen in hereditary nonpolyposis colorectal cancer (HNPCC), and patients with MSI-high tumors tend to have a better prognosis. MSI status is important for selecting patients who may benefit from immune checkpoint inhibitors.
Step 3: Role in Treatment and Prognosis:
MSI-high tumors are more likely to respond to immune checkpoint inhibitors like pembrolizumab, making MSI testing essential in the management of colorectal cancer. Quick Tip: MSI testing is increasingly used to guide treatment decisions, particularly in the context of immunotherapy for colorectal cancer.
Management of metastatic RCC.
View Solution
Renal cell carcinoma (RCC) is a malignancy of the kidney that can metastasize to various organs. The management of metastatic RCC (mRCC) requires a multi-disciplinary approach, involving systemic therapies, targeted therapies, and sometimes surgical intervention.
Step 1: Systemic Therapy:
The mainstay of treatment for mRCC includes targeted therapies, such as tyrosine kinase inhibitors (TKIs) like sunitinib and pazopanib, and immune checkpoint inhibitors like nivolumab and pembrolizumab. These therapies work by inhibiting angiogenesis and promoting immune-mediated tumor destruction.
Step 2: Immunotherapy:
Immunotherapy has become a cornerstone in the management of mRCC. Combination therapies, such as nivolumab and ipilimumab, have shown improved survival rates in patients with mRCC by enhancing the body's immune response to the tumor.
Step 3: Surgical Management:
Surgical resection of metastatic lesions may be considered in select patients, especially if they have a limited number of metastatic sites. Nephrectomy (removal of the primary tumor) is also part of the management for certain patients. Quick Tip: Immune checkpoint inhibitors and targeted therapies have significantly improved the prognosis for patients with metastatic RCC.
Management of glioblastoma multiforme.
View Solution
Glioblastoma multiforme (GBM) is an aggressive form of brain cancer that requires a multimodal approach for management, including surgery, radiation, and chemotherapy.
Step 1: Surgical Management:
Surgical resection is the primary treatment for glioblastoma, aiming to remove as much of the tumor as possible while preserving neurological function. However, complete resection is often not feasible due to the infiltrative nature of the tumor.
Step 2: Radiation Therapy:
Postoperative radiation therapy is typically recommended to treat any remaining tumor cells. The standard regimen involves fractionated radiation therapy, often delivered over six weeks.
Step 3: Chemotherapy:
Chemotherapy with temozolomide (TMZ) is commonly used alongside radiation. TMZ is an oral alkylating agent that has been shown to improve survival in patients with glioblastoma.
Step 4: Targeted and Immunotherapy:
Recent advances in molecular biology have led to the exploration of targeted therapies and immunotherapy for glioblastoma. These treatments aim to address the genetic mutations that drive the tumor's growth, but they are still in the experimental stages. Quick Tip: Treatment of glioblastoma multiforme involves a combination of surgery, radiation, and chemotherapy, with targeted therapies being explored in clinical trials.
Management of primary CNS lymphoma in the elderly.
View Solution
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive cancer that arises in the brain, spinal cord, or eye. Treatment in elderly patients requires careful consideration due to age-related factors and comorbidities.
Step 1: Chemotherapy:
Chemotherapy, often with high-dose methotrexate, is the cornerstone of treatment for PCNSL. Methotrexate is typically used in combination with other agents to achieve better tumor control.
Step 2: Radiation Therapy:
In elderly patients, radiation therapy may be used, but its role is limited due to potential neurocognitive side effects. Whole-brain radiation is sometimes considered for patients who are not candidates for chemotherapy or have residual disease after chemotherapy.
Step 3: Steroid Therapy:
Steroids are often used as part of the initial management to reduce inflammation and symptoms. However, their long-term use can lead to complications like immunosuppression, which must be managed carefully.
Step 4: Supportive Care:
Supportive care is critical for elderly patients, focusing on managing side effects, improving quality of life, and providing symptom relief. Palliative care is an option if the disease progresses or if the patient cannot tolerate aggressive treatments. Quick Tip: Treatment of primary CNS lymphoma in the elderly typically involves chemotherapy, with careful management of radiation and steroid use due to age-related factors.
Management of high risk GTN.
View Solution
Gestational Trophoblastic Neoplasia (GTN) is a group of rare diseases that arise from the cells that would normally form the placenta during pregnancy. High-risk GTN refers to cases where the cancer is aggressive or resistant to treatment. Proper management is critical to improving outcomes.
Step 1: Diagnosis of High-Risk GTN:
1. Clinical Presentation: High-risk GTN often presents with abnormal bleeding, elevated beta-hCG levels, and a history of molar pregnancy, abortion, or normal pregnancy.
2. Imaging and Histopathology: Ultrasound, CT scans, and biopsy are used to assess the extent of the disease and identify metastases.
3. Risk Scoring: The FIGO (International Federation of Gynecology and Obstetrics) scoring system is used to classify the risk based on the patient's clinical status.
Step 2: Treatment Approach:
1. Chemotherapy: The first-line treatment for high-risk GTN is chemotherapy, typically with a combination of methotrexate and dactinomycin. For resistant cases, additional agents such as etoposide or cisplatin may be used.
2. Surgical Intervention: In some cases, surgery (e.g., hysterectomy) may be necessary if chemotherapy is not effective.
3. Radiation Therapy: This may be used in cases where there is localized metastasis, particularly in the brain or lungs.
Step 3: Monitoring and Follow-Up:
Frequent monitoring of beta-hCG levels is essential during and after treatment to assess the response to therapy and detect any recurrence. Quick Tip: High-risk GTN requires aggressive treatment with chemotherapy and close monitoring to improve the chances of successful remission.
Prognostic score in GTN.
View Solution
The prognosis of Gestational Trophoblastic Neoplasia (GTN) is assessed using a scoring system that helps predict the likelihood of disease progression and the success of treatment. The most widely used scoring system is the FIGO (International Federation of Gynecology and Obstetrics) scoring system.
Step 1: The FIGO Scoring System:
1. Criteria: The FIGO score is based on the following factors: age of the patient, interval from the index pregnancy, pre-treatment serum beta-hCG levels, size and site of the tumor, and the presence of metastasis.
2. Risk Stratification: The total score classifies patients into low-risk and high-risk categories. A higher score indicates a greater risk of resistance to treatment and poorer prognosis.
Step 2: High-Risk Prognostic Factors:
1. High beta-hCG levels: Extremely elevated beta-hCG levels are associated with a worse prognosis.
2. Metastatic Disease: The presence of metastasis to vital organs such as the lungs, liver, or brain is associated with a higher risk.
3. Large tumor size: Larger tumors tend to be more resistant to treatment and are linked to a poorer prognosis.
Step 3: Treatment and Follow-Up:
Prognostic scoring helps determine the appropriate treatment approach and frequency of monitoring. Patients with high-risk scores require more aggressive treatment, often with a combination of chemotherapy and other modalities. Quick Tip: The FIGO scoring system is essential in predicting the prognosis of GTN, helping clinicians tailor the treatment and follow-up for each patient.
Role of MSI in carcinoma colon.
View Solution
Microsatellite instability (MSI) is a condition of genetic hypermutability that occurs when the DNA mismatch repair (MMR) system is defective. In colon carcinoma, MSI plays a crucial role in tumorigenesis and is a marker for prognosis and therapy response.
Step 1: Mechanism of MSI in Colon Carcinoma:
MSI occurs when there are defects in the MMR system, leading to an accumulation of mutations in microsatellites, which are short, repetitive sequences of DNA. This can result in the activation of oncogenes or the inactivation of tumor suppressor genes.
Step 2: Clinical Implications:
MSI is often seen in hereditary nonpolyposis colorectal cancer (HNPCC), and patients with MSI-high tumors tend to have a better prognosis. MSI status is important for selecting patients who may benefit from immune checkpoint inhibitors.
Step 3: Role in Treatment and Prognosis:
MSI-high tumors are more likely to respond to immune checkpoint inhibitors like pembrolizumab, making MSI testing essential in the management of colorectal cancer. Quick Tip: MSI testing is increasingly used to guide treatment decisions, particularly in the context of immunotherapy for colorectal cancer.
Management of metastatic RCC.
View Solution
Renal cell carcinoma (RCC) is a malignancy of the kidney that can metastasize to various organs. The management of metastatic RCC (mRCC) requires a multi-disciplinary approach, involving systemic therapies, targeted therapies, and sometimes surgical intervention.
Step 1: Systemic Therapy:
The mainstay of treatment for mRCC includes targeted therapies, such as tyrosine kinase inhibitors (TKIs) like sunitinib and pazopanib, and immune checkpoint inhibitors like nivolumab and pembrolizumab. These therapies work by inhibiting angiogenesis and promoting immune-mediated tumor destruction.
Step 2: Immunotherapy:
Immunotherapy has become a cornerstone in the management of mRCC. Combination therapies, such as nivolumab and ipilimumab, have shown improved survival rates in patients with mRCC by enhancing the body's immune response to the tumor.
Step 3: Surgical Management:
Surgical resection of metastatic lesions may be considered in select patients, especially if they have a limited number of metastatic sites. Nephrectomy (removal of the primary tumor) is also part of the management for certain patients. Quick Tip: Immune checkpoint inhibitors and targeted therapies have significantly improved the prognosis for patients with metastatic RCC.




Comments